Past Webinar
Seeded Aggregation and Transmissible Proteopathy—Creepy Stuff Not Just for Prions Anymore?
Quick Links
Introduction
The pathologic similarities between prion diseases and other disorders involving protein aggregation have been apparent for decades, but it has been generally thought that only prion disease can be propagated by corruptive protein seeding. A spate of recent findings—some quite surprising—indicate that the seeded induction of aggregation is possible, albeit with varying degrees of efficiency, for a growing variety of pathogenic proteins, including Aβ, tau, α-synuclein, huntingtin, and—outside of the brain—amyloid A and apolipoprotein A-II. If seeded protein misfolding and assembly indeed is a common mechanism of pathogenesis, this would have important implications not only for understanding how diverse disorders begin, but also for how proteopathy spreads from cell to cell, and tissue to tissue.
This Webinar, led by Lary Walker, explored these questions and more:
- What are the similarities among aggregating proteins, what are the differences?
- How is the prion model of transmissible proteopathy applicable to the induction of other proteopathies? How is it not?
- By which molecular mechanisms do seeds induce proteins to misfold and aggregate?
- What are the mechanisms of disease spread?
- What features of the protein assemblies and host are necessary for the seeded induction? Are these conditions similar for all pathogenic proteins?
- Do all pathogenic proteins have the capability to form polystructural/polyfunctional strains? What is the nature of the strains?
- To what extent can heterologous molecules precipitate protein aggregation?
- Are there potential public health implications of protein seeding that we should begin to consider for AD/PD/HD?
- Medical procedures—brain surgery?
- Dietary factors
- Nanotechnology
As always, your comments and questions are welcome. See the background text for this webinar below.
- View/Listen to the Webinar
Click on this image to launch the recording.
Background
Dense protein aggregates formed from misfolded protein monomers are a feature of many neurodegenerative diseases, including Alzheimer, Parkinson, and Huntington diseases, amyotrophic lateral sclerosis (ALS), and prion diseases, such as Creutzfeldt-Jakob disease. Protein aggregation is also a facet of non-neurodegenerative diseases, such as systemic amyloid A amyloidosis. Of all these disorders, the prion diseases are unique because pathogenic prion proteins are infectious agents that seed the misfolding of normal prion protein and its subsequent aggregation in normal cells and organisms. Different protein conformations, or strains, of prions can also cause disease characteristics or phenotypes (Collinge et al., 2007).
But are prions truly unique in this? A flurry of recent research suggests otherwise. Though misfolded amyloidβ (Aβ), α-synuclein, huntingtin, and other aggregation-prone proteins may not be infectious agents in the sense that they spread disease from one person to the next, evidence has grown that within an individual organism, misfolded forms of these proteins spread through cells and tissues, corrupting normal proteins and seeding protein aggregation as they go. If this is a common mechanism for the spread of pathogenic proteins in a given person, it would have profound implications for the study and treatment of neurodegenerative diseases.
Amyloid-β
Early evidence that non-prion proteins may seed protein aggregation in vivo came from Lary Walker’s lab at Emory University, Atlanta, Georgia. Walker and colleagues showed that Alzheimer disease brain extracts infused into young APP mice could precipitate protein aggregation five months later (Kane et al., 2001). In primates, too, seeding with Aβ-laden brain extracts increases the likelihood that amyloid plaques will develop with age (Ridley et al., 2006). More recently, Mathias Jucker, Hertie Institute for Clinical Brain Research in Tubingen, Germany, and colleagues showed that when injected into discrete locations in the brain of young APP23 mice, diluted extracts from aged APP23 transgenic mice can induce plaque formation near the injection site within three months, and that the pathology spreads to more distal regions by six months (see ARF news on Eisele et al., 2009). The finding supports the idea that Aβ seeds can diffuse and corrupt normal protein in the brain. Earlier, Jucker and colleagues also reported that the type of plaque induced by brain extracts depends not only the type of Aβ in the extract, but also on the nature of the Aβ in the host. Extracts from APP/PS1 transgenic mice produce coarser, more punctate Aβ deposits in APP23 mice, whereas extracts from APP23 mice cause more diffuse plaques in these animals. These phenotypes may depend on the relative amounts of Aβ40 and Aβ42 in the donors and hosts. This would seem to support the idea that, like with prions, there can be different “strains” of Aβ (see ARF related news on Meyer-Luehmann et al., 2006). Fluctuating Aβ40/42 ratios may even be linked to regional brain differences in plaque morphology.
Tau, Too?
This year, strong evidence for the seeding and propagation of the microtubule protein tau also emerged. At the cellular level, Marc Diamond, now at Washington University, St. Louis, Missouri, and colleagues showed that tau, even though it is an intracellular protein, forms seeds that can be passed from one cell to the next, where the seeds induce aggregation of normal tau (see ARF related news on Frost et al., 2009). Tau seeding also occurs in vivo, according to work from the labs of Markus Tolnay at the University of Basel, Switzerland and Michel Goedert MRC Laboratory of Molecular Biology, Cambridge, UK. They showed that brain extracts from P301S tau transgenic mice, which produce filamentous tau aggregates, can induce tau aggregation in another tau-overexpressing mouse strain (ALZ17 mice) that do not normally make tau filaments. Tau aggregates in the ALZ17 mice took six months to appear, and they grew further over the next 6 – 8 months. Importantly, the aggregates spread from the injection site to connected sites in the brain, hinting that the spread of tau pathology in human disease may follow neuronal circuits. Interestingly, Diamond’s work suggests that tau, too, occurs in at least two conformations, or strains, that differ in secondary structure. Seeding with mutant tau drives wild-type (WT) tau into a secondary structure that Diamond calls WT*.
Huntingtin and α-synuclein
The prion-like creep of protein aggregates in the brain is not limited to Alzheimer disease. Mutant huntingtin and α-synuclein may spread in a similar fashion in Huntington and Parkinson diseases, respectively. Ron Kopito’s lab at Stanford University, California, showed that huntingtin-like protein fragments with expanded polyglutamine stretches (Q44) can gain entry into cells and seed aggregation of normal-length (Q25) peptides (see ARF news and Ren et al., 2009). The spread and induction of α-synuclein from one cell to another in vitro was recently described by researchers led by Seung-Jae Lee, Konkuk University in Seoul, South Korea and by Eliezer Masliah, University of California at San Diego (see related ARF news on Desplats et al., 2009). These investigators further showed that normal stem cells transplanted into mutant α-synuclein transgenic mice also acquired the mutant protein, suggesting that cell-to-cell transfer occurs in vivo. This experiment might help explain why normal cell grafts transplanted into the brain of Parkinson’s patients succumbed to Parkinson pathology years later (see related ARF news).
Outside the brain, prion-like mechanisms are known to occur, for example, in systemic amyloidoses. Amyloid A (AA) fibrils can induce AA aggregation when injected into mice (see Lundmark et al., 2002), as can fibrils of apolipoprotein AII (see Xing et al., 2001).
Selected Reviews on Seeding of Proteopathy:
Aguzzi A, Baumann F, Bremer J. The prion's elusive reason for being. Annu Rev Neurosci. 2008;31:439-77. Abstract
Collinge J, Clarke AR. A general model of prion strains and their pathogenicity. Science. 2007 Nov 9;318(5852):930-6. Abstract
Frost B, Diamond MI. The expanding realm of prion phenomena in neurodegenerative disease. Prion. 2009 Apr;3(2):74-7. Abstract
Lansbury PT. Structural neurology: are seeds at the root of neuronal degeneration? Neuron. 1997 Dec;19(6):1151-4. Abstract
Sigurdsson EM, Wisniewski T, Frangione B. Infectivity of amyloid diseases. Trends Mol Med. 2002 Sep;8(9):411-3. Abstract
Soto C, Estrada L, Castilla J. Amyloids, prions and the inherent infectious nature of misfolded protein aggregates. Trends Biochem Sci. 2006 Mar;31(3):150-5. Abstract
Walker LC, Levine H, Mattson MP, Jucker M. Inducible proteopathies. Trends Neurosci. 2006 Aug;29(8):438-43. Abstract
Selected Primary Papers on Seeding:
Bolmont T, Clavaguera F, Meyer-Luehmann M, Herzig MC, Radde R, Staufenbiel M, Lewis J, Hutton M, Tolnay M, Jucker M. Induction of tau pathology by intracerebral infusion of amyloid-beta -containing brain extract and by amyloid-beta deposition in APP x Tau transgenic mice. Am J Pathol. 2007 Dec;171(6):2012-20. Abstract
Clavaguera F, Bolmont T, Crowther RA, Abramowski D, Frank S, Probst A, Fraser G, Stalder AK, Beibel M, Staufenbiel M, Jucker M, Goedert M, Tolnay M. Transmission and spreading of tauopathy in transgenic mouse brain. Nat Cell Biol. 2009 Jul;11(7):909-13. Abstract
Desplats P, Lee HJ, Bae EJ, Patrick C, Rockenstein E, Crews L, Spencer B, Masliah E, Lee SJ. Inclusion formation and neuronal cell death through neuron-to-neuron transmission of alpha-synuclein. Proc Natl Acad Sci U S A. 2009 Aug 4;106(31):13010-5. Abstract
Eisele YS, Bolmont T, Heikenwalder M, Langer F, Jacobson LH, Yan ZX, Roth K, Aguzzi A, Staufenbiel M, Walker LC, Jucker M. Induction of cerebral beta-amyloidosis: intracerebral versus systemic Abeta inoculation. Proc Natl Acad Sci U S A. 2009 Aug 4;106(31):12926-31. Abstract
Fu X, Korenaga T, Fu L, Xing Y, Guo Z, Matsushita T, Hosokawa M, Naiki H, Baba S, Kawata Y, Ikeda S, Ishihara T, Mori M, Higuchi K. Induction of AApoAII amyloidosis by various heterogeneous amyloid fibrils. FEBS Lett. 2004 Apr 9;563(1-3):179-84. Abstract
Gaspar RC, Villarreal SA, Bowles N, Hepler RW, Joyce JG, Shughrue PJ. Oligomers of beta-amyloid are sequestered into and seed plaques in the brains of an AD mouse model. Exp Neurol. 2009 Sep 8; Abstract
Götz J, Chen F, Van Dorpe J, Nitsch RM. Formation of neurofibrillary tangles in P301l tau transgenic mice induced by Abeta 42 fibrils. Science. 2001 Aug 24;293(5534):1491-5. Abstract
Kane MD, Lipinski WJ, Callahan MJ, Bian F, Durham RA, Schwarz RD, Roher AE, Walker LC. Evidence for seeding of beta -amyloid by intracerebral infusion of Alzheimer brain extracts in beta -amyloid precursor protein-transgenic mice. J Neurosci. 2000 May 15;20(10):3606-11. Abstract
Legname G, Baskakov IV, Nguyen HO, Riesner D, Cohen FE, Dearmond SJ, Prusiner SB. Synthetic mammalian prions. Science. 2004 Jul 30;305(5684):673-6. Abstract
Lundmark K, Westermark GT, Nyström S, Murphy CL, Solomon A, Westermark P. Transmissibility of systemic amyloidosis by a prion-like mechanism. Proc Natl Acad Sci U S A. 2002 May 14;99(10):6979-84. Abstract
Lundmark K, Westermark GT, Olsén A, Westermark P. Protein fibrils in nature can enhance amyloid protein A amyloidosis in mice: Cross-seeding as a disease mechanism. Proc Natl Acad Sci U S A. 2005 Apr 26;102(17):6098-102. Abstract
Meyer-Luehmann M, Coomaraswamy J, Bolmont T, Kaeser S, Schaefer C, Kilger E, Neuenschwander A, Abramowski D, Frey P, Jaton AL, Vigouret JM, Paganetti P, Walsh DM, Mathews PM, Ghiso J, Staufenbiel M, Walker LC, Jucker M. Exogenous induction of cerebral beta-amyloidogenesis is governed by agent and host. Science. 2006 Sep 22;313(5794):1781-4. Abstract
Petkova AT, Leapman RD, Guo Z, Yau WM, Mattson MP, Tycko R. Self-propagating, molecular-level polymorphism in Alzheimer's beta-amyloid fibrils. Science. 2005 Jan 14;307(5707):262-5. Abstract
Ren PH, Lauckner JE, Kachirskaia I, Heuser JE, Melki R, Kopito RR. Cytoplasmic penetration and persistent infection of mammalian cells by polyglutamine aggregates. Nat Cell Biol. 2009 Feb;11(2):219-25. Abstract
Ridley RM, Baker HF, Windle CP, Cummings RM. Very long term studies of the seeding of beta-amyloidosis in primates. J Neural Transm. 2006 Sep;113(9):1243-51. Abstract
Solomon A, Richey T, Murphy CL, Weiss DT, Wall JS, Westermark GT, Westermark P. Amyloidogenic potential of foie gras. Proc Natl Acad Sci U S A. 2007 Jun 26;104(26):10998-1001. Abstract
Vande Velde C, Miller TM, Cashman NR, Cleveland DW. Selective association of misfolded ALS-linked mutant SOD1 with the cytoplasmic face of mitochondria. Proc Natl Acad Sci U S A. 2008 Mar 11;105(10):4022-7. Abstract
Westermark P, Lundmark K, Westermark GT. Fibrils from designed non-amyloid-related synthetic peptides induce AA-amyloidosis during inflammation in an animal model. PLoS One. 2009;4(6):e6041.Abstract
Xing Y, Nakamura A, Chiba T, Kogishi K, Matsushita T, Li F, Guo Z, Hosokawa M, Mori M, Higuchi K. Transmission of mouse senile amyloidosis. Lab Invest. 2001 Apr;81(4):493-9. Abstract
Zhang B, Une Y, Fu X, Yan J, Ge F, Yao J, Sawashita J, Mori M, Tomozawa H, Kametani F, Higuchi K. Fecal transmission of AA amyloidosis in the cheetah contributes to high incidence of disease. Proc Natl Acad Sci U S A. 2008 May 20;105(20):7263-8. Abstract
Zhou Z, Fan JB, Zhu HL, Shewmaker F, Yan X, Chen X, Chen J, Xiao GF, Guo L, Liang Y. Crowded, Cell-like Environment Accelerates the Nucleation Step of Amyloidogenic Protein Misfolding. J Biol Chem. 2009 Sep 10; Abstract
References
News Citations
- Aβ the Bad Apple? Seeding and Propagating Amyloidosis
- Double Paper Alert—A Function for BACE, a Basis for Amyloid
- Keystone: Tau, Huntingtin—Do Prion-like Properties Play a Role in Disease?
- Research Brief: α-synuclein Spoils the Neural Neighborhood
- Dopaminergic Transplants—Stable But Prone to Parkinson’s?
Paper Citations
- Kane MD, Lipinski WJ, Callahan MJ, Bian F, Durham RA, Schwarz RD, Roher AE, Walker LC. Evidence for seeding of beta -amyloid by intracerebral infusion of Alzheimer brain extracts in beta -amyloid precursor protein-transgenic mice. J Neurosci. 2000 May 15;20(10):3606-11. PubMed.
- Ridley RM, Baker HF, Windle CP, Cummings RM. Very long term studies of the seeding of beta-amyloidosis in primates. J Neural Transm. 2006 Sep;113(9):1243-51. PubMed.
- Eisele YS, Bolmont T, Heikenwalder M, Langer F, Jacobson LH, Yan ZX, Roth K, Aguzzi A, Staufenbiel M, Walker LC, Jucker M. Induction of cerebral beta-amyloidosis: intracerebral versus systemic Abeta inoculation. Proc Natl Acad Sci U S A. 2009 Aug 4;106(31):12926-31. PubMed.
- Meyer-Luehmann M, Coomaraswamy J, Bolmont T, Kaeser S, Schaefer C, Kilger E, Neuenschwander A, Abramowski D, Frey P, Jaton AL, Vigouret JM, Paganetti P, Walsh DM, Mathews PM, Ghiso J, Staufenbiel M, Walker LC, Jucker M. Exogenous induction of cerebral beta-amyloidogenesis is governed by agent and host. Science. 2006 Sep 22;313(5794):1781-4. PubMed.
- Frost B, Jacks RL, Diamond MI. Propagation of tau misfolding from the outside to the inside of a cell. J Biol Chem. 2009 May 8;284(19):12845-52. PubMed.
- Ren PH, Lauckner JE, Kachirskaia I, Heuser JE, Melki R, Kopito RR. Cytoplasmic penetration and persistent infection of mammalian cells by polyglutamine aggregates. Nat Cell Biol. 2009 Feb;11(2):219-25. PubMed.
- Desplats P, Lee HJ, Bae EJ, Patrick C, Rockenstein E, Crews L, Spencer B, Masliah E, Lee SJ. Inclusion formation and neuronal cell death through neuron-to-neuron transmission of alpha-synuclein. Proc Natl Acad Sci U S A. 2009 Aug 4;106(31):13010-5. PubMed.
- Lundmark K, Westermark GT, Nyström S, Murphy CL, Solomon A, Westermark P. Transmissibility of systemic amyloidosis by a prion-like mechanism. Proc Natl Acad Sci U S A. 2002 May 14;99(10):6979-84. PubMed.
- Xing Y, Nakamura A, Chiba T, Kogishi K, Matsushita T, Li F, Guo Z, Hosokawa M, Mori M, Higuchi K. Transmission of mouse senile amyloidosis. Lab Invest. 2001 Apr;81(4):493-9. PubMed.
- Frost B, Diamond MI. The expanding realm of prion phenomena in neurodegenerative disease. Prion. 2009 Apr-Jun;3(2):74-7. PubMed.
- Lansbury PT. Structural neurology: are seeds at the root of neuronal degeneration?. Neuron. 1997 Dec;19(6):1151-4. PubMed.
- Sigurdsson EM, Wisniewski T, Frangione B. Infectivity of amyloid diseases. Trends Mol Med. 2002 Sep;8(9):411-3. PubMed.
- Soto C, Estrada L, Castilla J. Amyloids, prions and the inherent infectious nature of misfolded protein aggregates. Trends Biochem Sci. 2006 Mar;31(3):150-5. PubMed.
- Walker LC, Levine H, Mattson MP, Jucker M. Inducible proteopathies. Trends Neurosci. 2006 Aug;29(8):438-43. PubMed.
- Bolmont T, Clavaguera F, Meyer-Luehmann M, Herzig MC, Radde R, Staufenbiel M, Lewis J, Hutton M, Tolnay M, Jucker M. Induction of tau pathology by intracerebral infusion of amyloid-beta -containing brain extract and by amyloid-beta deposition in APP x Tau transgenic mice. Am J Pathol. 2007 Dec;171(6):2012-20. PubMed.
- Clavaguera F, Bolmont T, Crowther RA, Abramowski D, Frank S, Probst A, Fraser G, Stalder AK, Beibel M, Staufenbiel M, Jucker M, Goedert M, Tolnay M. Transmission and spreading of tauopathy in transgenic mouse brain. Nat Cell Biol. 2009 Jul;11(7):909-13. PubMed.
- Fu X, Korenaga T, Fu L, Xing Y, Guo Z, Matsushita T, Hosokawa M, Naiki H, Baba S, Kawata Y, Ikeda S, Ishihara T, Mori M, Higuchi K. Induction of AApoAII amyloidosis by various heterogeneous amyloid fibrils. FEBS Lett. 2004 Apr 9;563(1-3):179-84. PubMed.
- Gaspar RC, Villarreal SA, Bowles N, Hepler RW, Joyce JG, Shughrue PJ. Oligomers of beta-amyloid are sequestered into and seed new plaques in the brains of an AD mouse model. Exp Neurol. 2010 Jun;223(2):394-400. PubMed.
- Götz J, Chen F, van Dorpe J, Nitsch RM. Formation of neurofibrillary tangles in P301l tau transgenic mice induced by Abeta 42 fibrils. Science. 2001 Aug 24;293(5534):1491-5. PubMed.
- Legname G, Baskakov IV, Nguyen HO, Riesner D, Cohen FE, Dearmond SJ, Prusiner SB. Synthetic mammalian prions. Science. 2004 Jul 30;305(5684):673-6. PubMed.
- Lundmark K, Westermark GT, Olsén A, Westermark P. Protein fibrils in nature can enhance amyloid protein A amyloidosis in mice: Cross-seeding as a disease mechanism. Proc Natl Acad Sci U S A. 2005 Apr 26;102(17):6098-102. PubMed.
- Petkova AT, Leapman RD, Guo Z, Yau WM, Mattson MP, Tycko R. Self-propagating, molecular-level polymorphism in Alzheimer's beta-amyloid fibrils. Science. 2005 Jan 14;307(5707):262-5. PubMed.
- Solomon A, Richey T, Murphy CL, Weiss DT, Wall JS, Westermark GT, Westermark P. Amyloidogenic potential of foie gras. Proc Natl Acad Sci U S A. 2007 Jun 26;104(26):10998-1001. PubMed.
- Westermark P, Lundmark K, Westermark GT. Fibrils from designed non-amyloid-related synthetic peptides induce AA-amyloidosis during inflammation in an animal model. PLoS One. 2009;4(6):e6041. PubMed.
- Zhang B, Une Y, Fu X, Yan J, Ge F, Yao J, Sawashita J, Mori M, Tomozawa H, Kametani F, Higuchi K. Fecal transmission of AA amyloidosis in the cheetah contributes to high incidence of disease. Proc Natl Acad Sci U S A. 2008 May 20;105(20):7263-8. PubMed.
- Zhou Z, Fan JB, Zhu HL, Shewmaker F, Yan X, Chen X, Chen J, Xiao GF, Guo L, Liang Y. Crowded cell-like environment accelerates the nucleation step of amyloidogenic protein misfolding. J Biol Chem. 2009 Oct 30;284(44):30148-58. PubMed.
External Citations
Further Reading
Papers
- Selkoe DJ. The origins of Alzheimer disease: a is for amyloid. JAMA. 2000 Mar 22-29;283(12):1615-7. PubMed.
- Näslund J, Haroutunian V, Mohs R, Davis KL, Davies P, Greengard P, Buxbaum JD. Correlation between elevated levels of amyloid beta-peptide in the brain and cognitive decline. JAMA. 2000 Mar 22-29;283(12):1571-7. PubMed.
- Olanow CW, Prusiner SB. Is Parkinson's disease a prion disorder?. Proc Natl Acad Sci U S A. 2009 Aug 4;106(31):12571-2. PubMed.
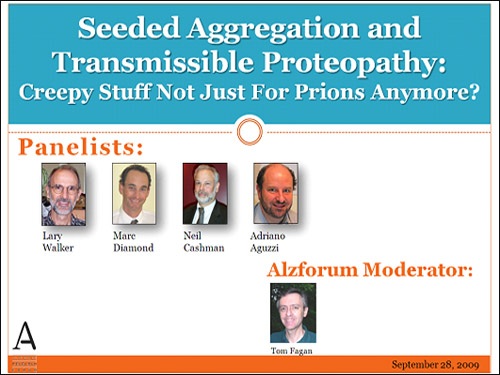
Panelists
-
 Lary Walker, Ph.D.
Emory University
Lary Walker, Ph.D.
Emory University
-
 Adriano Aguzzi
Adriano Aguzzi
-
 Neil Cashman, neil.cashman@vch.ca
UBC
Neil Cashman, neil.cashman@vch.ca
UBC
-
 Marc Diamond, MD
University of Texas, Southwestern Medical Center
Marc Diamond, MD
University of Texas, Southwestern Medical Center

Comments
Shinshu University Graduate School of Medicine
Transmissibility of Amyloidoses, Findings From Animal Models of Systemic Amyloidoses
Currently, more than 25 amyloid diseases have been identified. In mice, apolipoprotein AII (ApoAII) in serum high-density lipoproteins (HDL) forms amyloid fibrils in age-associated systemic amyloidosis (AApoAII amyloidosis). Serum amyloid A (SAA) protein in HDL forms amyloid fibrils in AA amyloidosis, which is generally recognized as the predominant form of systemic amyloidosis that occurs in humans, mice, and domestic animals. These amyloidoses are characterized by the systemic and extracellular deposition of amyloid primarily in the spleen, liver, heart, kidney, vessel walls, and to a lesser extent in other organs. AApoAII amyloidosis occurs sporadically and is associated with aging, while AA amyloidosis is secondary to chronic inflammation. However, recent intriguing data suggest that both AApoAII and AA amyloidosis could be transmitted by a prion-like infectious process through a seeding-nucleation mechanism. In these amyloidoses, AApoAII, and AA amyloid fibrils, abnormal forms of the host serum proteins (ApoAII and SAA) induce the conformational change of ApoAII and SAA to the AApoAII and AA fibrils and cause detectable phenotypes or diseases in the affected individual.
Intravenous, peripheral, and oral injection of AApoAII amyloid fibrils markedly accelerated amyloidosis in mice. We have also observed that young mice rapidly develop amyloidosis when they share cages with old mice with severe amyloid deposits (horizontal transmission), and offspring nursed by amyloidosis-affected mothers showed early development of amyloidosis (vertical transmission). The propagation of amyloidosis among mice probably occurred by consumption of AApoAII fibrils found in feces, saliva, and milk (Korenaga et al., 2006).
It has been shown that experimental murine AA amyloidosis can be enhanced by dietary ingestion of amyloid fibrils (Lundmark et al., 2002). We recently proposed that feces may be a transmission vehicle causing an increased incidence of AA amyloidosis in captive cheetah (Acinonyx jubatus) populations (Zhang et al., 2008; related Commentary, Caughey and Baron, 2008). We found that cheetah feces contained AA amyloid fibrils that were different from those of the liver with regard to molecular weight and shape and had greater transmissibility (a different strain of fibril). We have reported that the incidence of visceral AA amyloidosis is unexpectedly high in slaughtered cattle, and AA amyloid fibrils isolated from these cattle have amyloid-enhancing activity (Yoshida et al., 2009). Although there has been no evidence that these foods produce harmful effects on human health, food-associated hazards for the development of systemic amyloidosis cannot be ignored. On the basis of recent studies with animal models, the patients at risk for secondary induced AA amyloidosis should avoid ingesting foods that containing AEF-like activity.
References:
Korenaga T, Yan J, Sawashita J, Matsushita T, Naiki H, Hosokawa M, Mori M, Higuchi K, Fu X. Transmission of amyloidosis in offspring of mice with AApoAII amyloidosis. Am J Pathol. 2006 Mar;168(3):898-906. PubMed.
Lundmark K, Westermark GT, Nyström S, Murphy CL, Solomon A, Westermark P. Transmissibility of systemic amyloidosis by a prion-like mechanism. Proc Natl Acad Sci U S A. 2002 May 14;99(10):6979-84. PubMed.
Zhang B, Une Y, Fu X, Yan J, Ge F, Yao J, Sawashita J, Mori M, Tomozawa H, Kametani F, Higuchi K. Fecal transmission of AA amyloidosis in the cheetah contributes to high incidence of disease. Proc Natl Acad Sci U S A. 2008 May 20;105(20):7263-8. PubMed.
Caughey B, Baron GS. Are cheetahs on the run from prion-like amyloidosis?. Proc Natl Acad Sci U S A. 2008 May 20;105(20):7113-4. PubMed.
Yoshida T, Zhang P, Fu X, Higuchi K, Ikeda S. Slaughtered aged cattle might be one dietary source exhibiting amyloid enhancing factor activity. Amyloid. 2009 Mar;16(1):25-31. PubMed.
Hunter College
The hypothesis that extracellular aggregates of proteins other than prions can enter cells and cause protein aggregation in other cells is very intriguing. It could be one possible explanation for the appearance of Lewy pathology in neurons grafted into the brains of PD patients.
However, another possible explanation for this phenomenon is that chronically activated microglia/astrocytes at the affected brain sites progressively affect the grafted neurons. Neurotoxins produced chronically by these glia create a toxic microenvironment for neurons. Therefore, the microenvironment generated by inflammation could be the culprit as well.
I have some questions/comments on the experiments involving neuron-neuron transmission of protein aggregates other than prions:
1. Are aggregates of synuclein, tau, or HTT detected extracellularly in the brains of patients affected by these diseases?
2. In the neuron-neuron transmission studies, immunofluorescence shows co-localization, but does it demonstrate internalization? Could the aggregates be stuck at the cell surface?
3. Most of these studies involve overexpression of fusion proteins that include fluorescent proteins, such as GFP, with the protein of interest, tau, synuclein, HTT fragments. Does overexpression and/or the fluorescent protein affect the destiny of these aggregates? Can the studies be replicated with lower protein levels without fusions?
4. HTT is a very large protein, ~350kDa. Can the expression of a fragment (polyQ) of the protein replicate the physiological/disease process?
5. It is proposed that the aggregates are removed by lysosomes. The intralysosomal pH is around 5? What is the fate of aggregates at pH 5? Do they become solubilized at an acidic pH, or does the level of aggregation increase, therefore preventing degradation by cathepsins?
6. In the CNS tissue sections, it appears that “abnormal SOD1” staining is only intracellular. Is this true? Did you observe any of the “abnormal SOD1” staining to be extracellular in ALS patients? If not, how can it be transmitted from one cell to the other?
Wyeth Pharmaceuticals
Not being an expert in the field, I may be asking a naive question, but many of the properties of prions and prion-like proteins seem to me to resemble the properties of chaperones proteins or HSPs. Could the "purpose" of these prion proteins be early evolutional forms of chaperones? Could what we know about chaperones be used in formulating therapeutic approaches?
University of Kentucky
Several of the proteins that aggregate in sporadic neurodegenerative disease are classified as "natively disordered." Much of the sequence is likely to be exposed to solvent. Would these diseases be resistant to treatment with antibodies to disease-specific epitopes (excepting perhaps soluble oligomer epitopes)?
F. Hoffmann-La Roche AG
How do you define a disease epitope for misfolded proteins such as is done for SOD1? Is toxicity to neurons a good indicator?
Emory University
Reply to comment by James Bergey
The mammalian proteins that have been shown thus far to have prion-like properties—the ability to amplify abnormal forms, presumably by the process of corruptive templating—appear to be of multiple types, and their normal functions often are poorly understood. For example, tau protein stabilizes microtubules; APP, the precursor of Aβ, may be involved in cell-cell adhesion and synapse formation; apolipoprotein A2, in contrast, is a component of high-density lipoproteins. A role for chaperones in prion-like protein behavior has been fairly well studied in yeast (see, e.g., Romanova and Chernoff, 2009; Shorter and Lindquist, 2008). For a nice evolutionary view of protein folding and misfolding in general, I would also recommend the papers by Dobson (Dobson, 1999; Stefani and Dobson, 2003; Dobson, 2006). Chaperones play a critical role in maintaining proteostasis, and as such could represent a potential therapeutic target for proteopathic disorders.
References:
Romanova NV, Chernoff YO. Hsp104 and prion propagation. Protein Pept Lett. 2009;16(6):598-605. PubMed.
Shorter J, Lindquist S. Hsp104, Hsp70 and Hsp40 interplay regulates formation, growth and elimination of Sup35 prions. EMBO J. 2008 Oct 22;27(20):2712-24. PubMed.
Dobson CM. Protein misfolding, evolution and disease. Trends Biochem Sci. 1999 Sep;24(9):329-32. PubMed.
Stefani M, Dobson CM. Protein aggregation and aggregate toxicity: new insights into protein folding, misfolding diseases and biological evolution. J Mol Med (Berl). 2003 Nov;81(11):678-99. PubMed.
Dobson CM. Protein aggregation and its consequences for human disease. Protein Pept Lett. 2006;13(3):219-27. PubMed.
University of Texas, Southwestern Medical Center
Reply to comment by Maria Figueiredo-Pereira
Q: The hypothesis that extracellular aggregates of proteins other than prions can enter cells and cause protein aggregation in other cells is very intriguing. It could be one possible explanation for the appearance of Lewy pathology in neurons grafted into the brains of PD patients.
However, another possible explanation for this phenomenon is that chronically activated microglia/astrocytes at the affected brain sites progressively affect the grafted neurons. Neurotoxins produced chronically by these glia create a toxic microenvironment for neurons. Therefore, the microenvironment generated by inflammation could be the culprit as well.
A: This is possible, and may contribute to pathology. However, a recent paper in PNAS (see Desplats et al., 2009 and ARF related news story) indicates that host protein can transfer directly to engrafted cells. In this work, a Tg mouse overexpressing human synuclein received wild-type transplanted cells. These transplanted cells developed human synuclein Lewy bodies, which could not have derived merely from effects of the “toxic” environment.
Q: I have some questions/comments on the experiments involving neuron-neuron transmission of protein aggregates other than prions:
1. Are aggregates of synuclein, tau, or Htt detected extracellularly in the brains of patients affected by these diseases?
A: I am not aware of Htt being deposited in the extracellular space, although we are now interested in testing HD spinal fluid for the protein. Likewise, I don’t know about synuclein. Tau protein definitely deposits in the extracellular space as “ghost tangles,” and is also detected in increasing amounts in the CSF of AD patients as the disease progresses.
2. In the neuron-neuron transmission studies, immunofluorescence shows colocalization, but does it demonstrate internalization? Could the aggregates be stuck at the cell surface?
A: In our work, we were careful to use confocal microscopy to rule out the possibility that aggregates were located at the cell surface. As far as we can tell, they are internalized, and are on the same focal plane as intracellular proteins such as tubulin.
3. Most of these studies involve overexpression of fusion proteins that include fluorescent proteins, such as GFP, with the protein of interest, tau, synuclein, Htt fragments. Does overexpression and/or the fluorescent protein affect the destiny of these aggregates? Can the studies be replicated with lower protein levels without fusions?
A: All studies with fluorescent protein fusions are vulnerable to artifact. We are now pursuing further experiments with proteins that do not have the fluorescent protein fusions.
4. Htt is a very large protein, ~350 kDa. Can the expression of a fragment (polyQ) of the protein replicate the physiological/disease process?
A: There is evidence that full-length Htt is cleaved to produce N-terminal fragments containing polyQ domains. It is absolutely clear, however, that flanking peptide sequences affect protein folding (both to increase and decrease it), most likely via effects on intrinsic structure of the peptide, but also, almost certainly, based on mediating protein-protein interactions within the cell. Thus, studies that use only pure polyQ domains are not really studying the “physiology” of the normal polyQ protein, but are rather looking at more generic aggregation phenomena. In the case of Htt, the N-terminal fragment retains various regions that mediate protein interactions. It is impossible to know to what extent this replicates misfolding in the disease state until modifiers are identified that affect pathology derived both from the fragment and from the full-length protein.
5. It is proposed that the aggregates are removed by lysosomes. The intralysosomal pH is around 5? What is the fate of aggregates at pH 5? Do they become solubilized at an acidic pH, or does the level of aggregation increase, therefore preventing degradation by cathepsins?
A: Certain peptides, such as Aβ, have increased aggregation at a lower pH. I am not sure whether pH has been studied in relation to Htt aggregation.
References:
Desplats P, Lee HJ, Bae EJ, Patrick C, Rockenstein E, Crews L, Spencer B, Masliah E, Lee SJ. Inclusion formation and neuronal cell death through neuron-to-neuron transmission of alpha-synuclein. Proc Natl Acad Sci U S A. 2009 Aug 4;106(31):13010-5. PubMed.
Make a Comment
To make a comment you must login or register.