Technology for Patients: Purring Robots, Digital Data-Gathering
Quick Links
As technology becomes ever more part of modern life, researchers are exploring how it can help people with dementia. At a satellite conference held July 21 in Chicago, before the Alzheimer’s Association International Conference, speakers showcased the latest advancements in this field. Applications of technology fell into two broad categories: improving quality of life, and data-gathering and diagnosis.
- Do robot companions ease life for people with dementia?
- Monitoring systems gather continuous data, but they aren’t always used.
- Virtual reality maze spots navigation problems better than paper version.
Regarding the former, speakers claimed that robots can provide companionship for patients and a respite for caregivers, or even help patients with daily tasks. Most such robots remain in research use only, though one therapeutic model, the Paro baby harp seal, is commercially available and was on display at AAIC.
Regarding the latter, researchers said passive sensor technologies can gather more detailed behavioral data than traditional reports, and they presented digital diagnostic tests that appear to have greater sensitivity and real-world validity than paper-and-pencil methods. Data-gathering is more commercially advanced than robotics. Many devices and apps are available now, and trials are beginning to incorporate digital, continuous-outcome measures (May 2017 conference news).

Paro robot with its inventor, Takanori Shibata. [Courtesy of Gabrielle Strobel.]
“There’s been a profusion of technology in the areas of sensors, wearables, and mobile communications,” said Jeffrey Kaye of the Layton Aging and Alzheimer’s Disease Center at Oregon Health and Science University in Portland, Oregon. However, he noted that many technological applications remain mired at the pilot stage. Barriers to widespread adoption range from cost and insufficient evidence that they work, to rapid obsolescence and lack of standardization of many technical devices (Dec 2012 news series). Nonetheless, Alex Mihailidis of the University of Toronto told Alzforum that he expects technology for dementia patients to become more commercially available within the next five years.
Eva, Paro: Social Robotics Gain Acceptance
Perhaps no tech application generates as much fascination as robotics. These machines are still crude, a far cry from the sophisticated androids of film, but even simple machines could help people with dementia, speakers said. Dementia causes people to become isolated, depressed, agitated, and behaviorally challenged. Robots don’t run out of “patience,” and might make serviceable companions at later stages of the disease.
In Chicago, Jesus Favela of CICESE Research Center in Ensenada, Mexico, discussed a prototype social robot he calls Eva. Eva sits on a table, and somewhat resembles a diminutive, simplified R2-D2. A smart phone behind her? its? eyes lends Eva video capabilities, and a computer inside the body handles speech recognition. Favela designed Eva to deliver conversation, social stimulation, and distraction for users, as well as potentially to intervene with problem behaviors.
Favela and doctoral student Dagoberto Cruz tested Eva in a pilot study of 12 dementia patients, whose average age was 80 and MMSE 14. In initial sessions with the participants, Eva asked questions about what foods and music they liked, and noted their conversation style. The researchers used the information to develop a personalized profile for each participant, which facilitated future interactions. For example, Eva would pause longer when talking with chatty people to give them time to speak. In these sessions, Eva often entertained small groups of participants by playing their favorite music. Favela showed a video of Eva playing a song and suggesting the listeners stand up and dance, which they did. In later sessions, Eva initiated more free-ranging conversations, or engaged participants by asking them to complete popular sayings.
Eva also helped moderate behavior. In another video, an agitated patient got up and walked away from the session. Eva asked her to please stay, and the woman returned, telling her companion, “She asked me so nicely, I have to stay.” In some sessions, Eva led relaxation exercises, suggesting her listeners close their eyes and breathe slowly.

Participants with dementia talk with Eva. [Courtesy of Jesus Favela.]
Perhaps surprisingly to an audience of cognitively normal, naturally skeptical scientists, the participants in this small study appeared to accept the robot as a conversation partner. Favela said they remembered Eva from one session to the next, although they did not always remember its name, or when they last interacted with it. Participants interacted, smiled, and laughed more as sessions went on, Favela added.
Sometimes conversations broke down. For example, when several people spoke simultaneously, Eva could not follow. However, participants tolerated these lapses and did most of the work of getting the conversation back on track, Favela said.
Participants did not seem to notice Eva’s digital nature—or did they tease Eva? In one video, a group of women told Eva their favorite food was mangos. When the robot said it did not eat mango, one woman demanded, “Why would you not eat such a delicious food?” “Because I am a robot,” Eva replied, sparking gales of laughter. Favela told Alzforum that the participants seemed to shift between treating the robot as an object and giving it a personality. One woman often invited Eva to visit her hometown, promising to host the robot at her house and cook meals for it, Favela said.
Favela and Cruz are working on upgrading Eva’s capabilities to allow it to read physiological signs, such as heart rate and temperature, and to adapt to the mood of its conversation partners. He believes the robot could be programmed to perform simple behavioral interventions, such as telling a person who wakes up in the middle of the night that it is not time to get up. Favela hopes Eva will be commercially available in the future.
While Eva is evolving, the Paro robot is already in widespread commercial use. Takanori Shibata of the National Institute of Advanced Industrial Science and Technology in Tsukuba, Japan, spearheaded its development in 2002. Shibata told Alzforum he designed Paro to look like a harp seal because people have few expectations about how this animal might behave, and therefore accept the robot more readily than they would a mechanical dog or cat. In Chicago, a handful of Paros stuck out their noses and soft, furry heads on a high-traffic corner booth of the exhibit hall, and few who passed by it could resist petting it. Paro blinks its eyes, moves in response to touch, and chirps and purrs. When cuddled, it wraps its flippers around its handler and rests its head on his or her shoulder. Paro’s software allows it to modify its behavior in response to a person’s actions, for example learning what elicits positive interactions such as petting, and then repeating that behavior.
Paro is now in its ninth generation, and has been in use in Japan and Europe since 2003. The company offers three different versions: The white seal is the most interactive and popular model, the gray seal is sleepy and snuggly, and the tan seal moves slowly. Paro’s price tag is $6,400.
A number of small studies have found that interacting with Paro benefits dementia patients. In a randomized controlled trial, those who played with Paro reported feeling less lonely, and in a pilot study, nursing home residents with access to Paro appeared calmer and happier, with fewer instances of yelling, pacing, and anxious behavior (Robinson et al., 2013; Lane et al., 2016). Other studies report that treatment groups score lower on measures of stress and anxiety, and have lower blood pressure after interacting with Paro. In randomized controlled trials, treatment groups used less psychotropic and pain medicine than controls (Robinson et al., 2015; Jøranson et al., 2016; Petersen et al., 2017). In 2009, the U.S. Food and Drug Administration approved Paro as a class II neurological therapeutic device.
When Will Robot Aides Be Feasible?
Designing a robot that renders more than soothing pet services remains a formidable challenge, and some groups are working on it. For example, François Michaud of the University of Sherbrooke, Canada, envisions robots that monitor people with dementia at home and report problems to family.
Michaud first adapted Amazon’s Beam Plus telecommunications device, a monitor on wheels designed for audio and video phone calls. Besides adding computing power and sensors, Michaud also enabled the device to move around a room and return to its docking station as needed, using a program called Simultaneous Localization and Mapping. His robot has speech-recognition software and tracks faces and voices. It can monitor vital signs such as heart rate and temperature (Lepage et al., 2016; Laniel et al., 2017).
Michaud is currently testing whether this robot could monitor people with dementia at night. He is working to improve its software by adding the ability to recognize common actions and to infer what task a person might be trying to accomplish, for example making a cup of tea. Ideally, the robot could then suggest tips. Michaud will build in spatiotemporal episodic memory so the robot can learn from human behavior patterns. Robots need to have contextual awareness in order to engage in meaningful interaction with people, Michaud noted. His is at the prototype stage; its base technology runs at $2,000.
In Chicago, speakers discussed more challenges they need to overcome. For one thing, a person’s speech changes as his or her dementia progresses, making it more difficult for software to interpret. Autonomous robots raise potential ethical concerns—could they make decisions for their owners, taking away their agency? Mobile robots could fall over and hurt people. Even so, researchers at AAIC thought robotic aides hold promise, with a favorable cost/benefit ratio for people with dementia.
Stream of Continuous Data From Passive Monitoring
Unlike the field of robotics, tech monitoring is no longer in its infancy. Its goal is to collect information in the background, through seamless, invisible applications. “The most effective technology is the most passive,” Kaye noted. One such system is Emerald, developed at MIT. From a small white box mounted to the wall, Emerald emits radio waves and detects their reflection from nearby objects to map its environment. It uploads raw data to a server and uses machine-learning algorithms to extract information about a person’s movements, location, and sleep patterns. It can measure respiration based on the movement of a person’s chest.
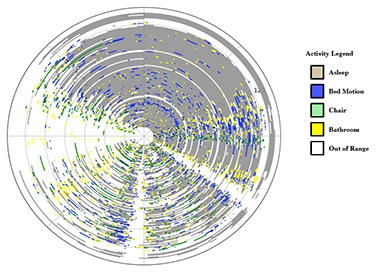
Daily Log.
Color-coded sensor data show how much time a 75-year-old study participant with vascular dementia, apathy, sleepiness, and anxiety spent in each activity. Circle represents 24 hours, concentric rings are separate days. [Courtesy of Ipsit Vahia.]
In a pilot study of how well Emerald gathers data on daily activities, Ipsit Vahia of McLean Hospital in Belmont, Massachusetts, installed it in the rooms of three volunteers in an assisted living center for four months. Emerald tracked pacing, walking speed, time spent in bed or in a chair, and sleep quality. Compared with observations by facility staff, Emerald generated more detailed data. Distinct patterns for each participant emerged, Vahia said at AAIC. Emerald identified sleep apnea, late-night waking and, in one case, showed that a participant became more agitated after having visitors. The data suggests Emerald could indeed spot behavioral changes and identify triggers for problem behavior, Vahia said.
But would nurses and aides use such data? Perhaps not so much. Katherine Wild, also at the Layton Aging and Alzheimer’s Disease Center, examined how well a similar passive monitoring system worked in retirement communities. Ninety-five residents in seven facilities participated for about two years each, and center staff could access the data via a computerized “dashboard.” The idea was that this might help caregivers decide when residents needed to move to a higher level of care. Alas, staff rarely logged in and did not use the data for decision-making, even though they had been involved in developing the dashboard. They told researchers there was too much data, and that it was difficult to differentiate acute events from trends. Some had trouble logging into the system, or had ethical qualms that viewing the data violated patient privacy. Overall, the technology was not sufficiently user-friendly, Wild concluded.

Virtual View. A VR maze combines the skills of real-world navigation and map-reading. [Courtesy of Raquel da Costa.]
Diagnostic Applications Gain Traction
Can technology improve diagnosis? Some digital measures are starting to trump older tests, speakers at AAIC agreed. For example, Raquel da Costa of the University of São Paulo noted that people with prodromal AD have trouble navigating through environments (Oct 2015 news; Jan 2017 news). Traditionally, researchers assess this deficit with the MRMT, aka Money Road-Map Test of Direction Sense, a paper-and-pencil test. However, looking at a two-dimensional map bears little resemblance to real-world navigating, so da Costa and colleagues wondered if a three-dimensional, virtual-reality maze would work better. Translating the MRMT into a VR experience, the research group developed the Spatial Orientation in an Immersive Virtual Environment Test (SOIVET) (da Costa et al., 2018).
To compare the two, da Costa enrolled 30 cognitively healthy people aged 18 to 59. Each completed the Santa Barbara Sense of Direction Scale survey to measure their own perception of how well they navigated. Then they took the MRMT as well as the virtual-reality version. For the latter, participants wore a headset giving them an immersive first-person view of a virtual world (see image). At their feet, they saw a two-dimensional map of their surroundings and used this information to find their way. In this way, the virtual-reality test mimicked real-world map-reading, requiring participants to split their attention between two tasks, da Costa said.
Participants found the virtual-reality task more difficult than the paper version, averaging 13 correct responses on the former versus 30 correct responses on the latter. Performance on the two tasks correlated with each other, suggested they measured the same skill. However, only the VR test score correlated with participants’ own sense of how well they could navigate; the MRMT did not correlate to the survey results. This suggests that the VR task better recreates real-world navigation and assesses spatial abilities more like those used in real life, da Costa said.
Other diagnostic tests use drawing to assess decline. A digital version of the clock-drawing task is already known to beat the paper-and-pen version (Aug 2018 conference news), and Kelvin Tsoi of the JC School of Public Health and Primary Care in Shatin, Hong Kong, described a different drawing test for which this appears to be true, as well. Noting that some dementia screening tests ask people to draw geometric shapes, Tsoi asked participants to draw two interlocking pentagons on a digital tablet while looking at a reference figure. Like the digital pen, the tablet measured factors such as drawing speed, hesitation, and stops at corners.
The researchers compared the performances of 194 AD patients seen at Hong Kong clinics to those of 271 cognitively healthy elderly recruited from community centers. The patients had an average age of 80, controls, 76. The former took an average 17.5 seconds to draw the shapes, compared with 12.6 seconds for controls. A machine learning algorithm predicted whether each participant had AD, based on his or her performance, and “diagnosed” AD with a sensitivity of 78 percent and specificity of 71 percent. Tsoi said that this beats the MMSE, which in this cohort had a sensitivity of 73 percent and specificity of 53 percent.
These talks but scratched the surface of technology research in AD. Other speakers noted advances in wearable technology, apps, and the design of “smart homes.” A key ingredient in taking these applications from research to real world will be to involve people with dementia in their design, speakers agreed.—Madolyn Bowman Rogers
References
News Citations
- Do Smartphones Collect Better Clinical Data Than Paper-and-Pencil Tests?
- Young ApoE4 Carriers Wander Off the ‘Grid’ — Early Predictor of Alzheimer’s?
- Led Astray: Pathology Tied to “Grid Cell” Malfunction in Tauopathy Model
- Weeklong Chinese Challenge Reveals Subtle Memory Problems
Series Citations
Paper Citations
- Robinson H, Macdonald B, Kerse N, Broadbent E. The psychosocial effects of a companion robot: a randomized controlled trial. J Am Med Dir Assoc. 2013 Sep;14(9):661-7. Epub 2013 Mar 30 PubMed.
- Lane GW, Noronha D, Rivera A, Craig K, Yee C, Mills B, Villanueva E. Effectiveness of a social robot, "Paro," in a VA long-term care setting. Psychol Serv. 2016 Aug;13(3):292-299. Epub 2016 May 19 PubMed.
- Robinson H, MacDonald B, Broadbent E. Physiological effects of a companion robot on blood pressure of older people in residential care facility: a pilot study. Australas J Ageing. 2015 Mar;34(1):27-32. Epub 2013 Dec 25 PubMed.
- Jøranson N, Pedersen I, Rokstad AM, Ihlebaek C. Change in quality of life in older people with dementia participating in Paro-activity: a cluster-randomized controlled trial. J Adv Nurs. 2016 Dec;72(12):3020-3033. Epub 2016 Aug 16 PubMed.
- Petersen S, Houston S, Qin H, Tague C, Studley J. The Utilization of Robotic Pets in Dementia Care. J Alzheimers Dis. 2017;55(2):569-574. PubMed.
- Lepage P, Letourneau D, Hamel M, Briere S, Corriveau H, Tousignant M, Michaud F. Telehomecare telecommunication framework - from remote patient monitoring to video visits and robot telepresence. Conf Proc IEEE Eng Med Biol Soc. 2016 Aug;2016:3269-3272. PubMed.
- Laniel S, Letourneau D, Labbe M, Grondin F, Polgar J, Michaud F. Adding navigation, artificial audition and vital sign monitoring capabilities to a telepresence mobile robot for remote home care applications. IEEE Int Conf Rehabil Robot. 2017 Jul;2017:809-811. PubMed.
- da Costa RQ, Pompeu JE, de Mello DD, Moretto E, Rodrigues FZ, Dos Santos MD, Nitrini R, Morganti F, Brucki SM. Two new virtual reality tasks for the assessment of spatial orientation Preliminary results of tolerability, sense of presence and usability. Dement Neuropsychol. 2018 Apr-Jun;12(2):196-204. PubMed.
Further Reading
Annotate
To make an annotation you must Login or Register.

Comments
AIST & Tokyo Institute of Technology
To add some information to this news article, Wendy Moyle and colleagues at Griffith University in Australia published a Cluster-RCT of PARO with 415 elderly people with dementia in the Journal of Post-Acute and Long-Term Care Medicine (Moyle et al., 2017).
PARO is an FDA-approved, non-pharmacological biofeedback medical device that has published clinical evidence. Therefore, Medicare and some private insurance companies in the U.S. accept reimbursement of prescribed treatments of therapy with PARO by using some CPT codes for anxiety, pain, depression, which can be used for patients with dementia.
References:
Moyle W, Jones CJ, Murfield JE, Thalib L, Beattie ER, Shum DK, O'Dwyer ST, Mervin MC, Draper BM. Use of a Robotic Seal as a Therapeutic Tool to Improve Dementia Symptoms: A Cluster-Randomized Controlled Trial. J Am Med Dir Assoc. 2017 Sep 1;18(9):766-773. Epub 2017 Aug 2 PubMed.
Make a Comment
To make a comment you must login or register.