Scientists Eager to Test ALS Gene Therapy
Quick Links
Researchers are eyeing a gene therapy they hope could eventually ameliorate most kinds of amyotrophic lateral sclerosis. A dose of up-frameshift protein 1 (UPF1) prevented degeneration in neuronal culture models of sporadic ALS, and versions due to TDP-43 or FUS mutations, according to a paper in the Proceedings of the National Academy of Sciences USA online June 8. Moreover, gene therapy in a rat ALS model produced startling improvement, preserving forelimb motility, as reported in the January Gene Therapy.
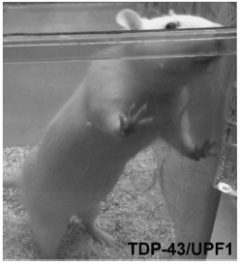
Rear and Reach.
ALS model rats treated with UPF1 maintained their forelimb strength. [Courtesy of Jackson et al., Gene Therapy]
“We are still not completely sure how it works,” said Gregory A. Petsko of the Weill Cornell Medical College in New York, who co-led the studies with Dagmar Ringe of Brandeis University in Waltham, Massachusetts. Right now, the authors are investigating the possibility that UPF1 bolsters the cell’s ability to dispose of nonsense mRNAs that contain premature stop codons. However, Petsko prioritizes finding a cure over understanding the mechanism fully, and has started negotiations with companies to develop the gene therapy further. “I think we have a reasonable chance that this is going to get tried out in people,” he said. In addition to ALS, frontotemporal dementia caused by TDP-43 or FUS pathology might be a disease target, Petsko said.
From Yeast to Neurons to Rats
It all started with a fungus. Shulin Ju, working with Ringe and Petsko, screened yeast for suppressors of FUS toxicity. Ju, who now runs his own lab at Wright State University in Dayton, Ohio, identified UPF1 as a powerful protector (see May 2011 news on Ju et al., 2011). UPF1 acts as a helicase to unwind RNA and regulates the destruction of RNAs containing nonsense codons; it also participates in RNA splicing and transport.
To test UPF1’s effects in a mammalian system, the authors struck up a collaboration with Sami Barmada in the laboratory of Steven Finkbeiner at the Gladstone Institutes in San Francisco. Finkbeiner’s lab uses automated microscopy to track the survival of individual neurons over time, allowing the researchers to calculate the risk of cell death for different treatments (see image below).

Another one bites the dust.
Researchers used automated microscopy to track cultured neurons over time, noting when each cell disappeared so they could calculate the overall risk of death. The red arrows indicate cells about to expire. [Courtesy of Barmada et al., PNAS]
As reported in the PNAS paper, Barmada transfected primary rat cortical neurons with wild-type TDP-43 and FUS, and mutant versions of each. Since TDP-43 accumulates in sporadic ALS, the authors believe these models represent both sporadic and genetic disease. To some cultures, he also added the gene for UPF1. “We saw a huge effect size,” said Barmada, who now runs a lab at the University of Michigan Medical School in Ann Arbor. UPF1 diminished the risk of cell death by 20 to 50 percent.
Petsko presented these data at a 2011 meeting in Arlington, Virginia (see Nov 2011 news). He said, “If anybody would like to try UPF1 in their TDP-43 or FUS model, come talk to me.” Up came Ronald Klein of the Louisiana State University Health Sciences Center in Shreveport, offering his rat model of TDP-43 disease. His lab employs adeno-associated virus (AAV) to deliver a wild-type human TDP-43 transgene to the rat spinal cord (see Mar 2009 news on Tatom et al., 2009; Wang et al., 2010). This reliably causes hindlimb paralysis in all rats, as well as forelimb paralysis in about 75 percent of animals, depending on the vector dosage, Klein told Alzforum.
Klein and Kasey Jackson, first author on the Gene Therapy paper, managed to stuff all 3.3 kilobases of UPF1 into AAV and inject it intravenously. When Jackson treated the first set of rats, she noticed a difference right away. As the rats moved around their cages, it was obvious which ones had received UPF1, because they walked better. In a battery of tests, they balanced better on a rotating rod, walked farther during a 30-minute period, and dangled longer from a wire mesh before falling. While their hindlimbs remained paralyzed, they could still reach with their forelimbs (see image above).
The researchers might be able to optimize the treatment to achieve hindlimb benefits, too, Petsko said. They can vary the dose of AAV, use a different virus strain, or deliver it directly to the nervous system instead of intravenously.
“These papers are a nice example of extension from a primary screen in yeast to modulation in neuronal cultures and an in vivo model,” commented Lawrence Hayward of the University of Massachusetts Medical School in Worcester, who was not involved in the work. He cautioned, “The potential limitations of overexpression model phenotypes should be kept in mind.”
Stuff of Nonsense
UPF1 rescues neurons and rats from the toxic effects of TDP-43 and FUS—but how? Barmada’s study offers some clues. Initially, the authors thought UPF1 might be a general promoter of neuron survival, but they found it made no difference to the death rate of control neurons. Neurons expressing a polyglutamate expansion or mutant human SOD1, another ALS gene, were similarly unaffected by extra UPF1. “This provides some of the first evidence that the SOD1 form of ALS is distinct, and will probably require distinct treatment strategies,” Petsko said.
UPF1 is a master regulator for nonsense-mediated decay (NMD), a known RNA surveillance mechanism that degrades unwanted RNAs. It gets rid of RNAs with nonsense codons that create premature stop sites, and also participates in the natural cycle of turnover for proper RNAs. Barmada and colleagues treated the cultures with the NMD inhibitor NMDI. This drug curtailed the survival of UPF1-treated neurons, suggesting UPF1 promotes survival, at least in part, by amplifying NMD.
As it happens, TDP-43 and FUS both inhibit their own RNAs, routing them toward NMD by creating alternate splice forms (see Jan 2011 news; Zhou et al., 2013; Polymenidou et al., 2011). Brian Freibum of St. Jude Children’s Research Hospital in Memphis, Tennessee, who was not involved in the research, commented that enhancing NMD of TDP-43 and FUS RNA, which would effectively downregulate the toxic proteins, is a likely explanation for the benefits Barmada and Jackson observed.
“The evidence is teasingly suggestive that UPF1 might work by NMD,” said Petsko, though he added that at this stage, “I would not rule anything out.” Barmada offered a second hypothesis, noting that TDP-43 and UPF1 are binding partners. The presence of additional copies of UPF1 from the gene therapy might sequester toxic TDP-43, he speculated. Alternatively, the cellular TDP-43 might grab and inhibit UPF1, but the added UPF1 could overcome this effect.—Amber Dance
References
News Citations
- Yeast Models Say TDP-43 and FUS Are Not Cut From the Same Cloth
- DC: ALS Treatment Possibilities Presented at SfN, Satellite
- TDP-43 Roundup: New Models, New Genes
- TDP-43 Turns Itself Off, Inclusions a False Lead
Paper Citations
- Ju S, Tardiff DF, Han H, Divya K, Zhong Q, Maquat LE, Bosco DA, Hayward LJ, Brown RH, Lindquist S, Ringe D, Petsko GA. A Yeast Model of FUS/TLS-Dependent Cytotoxicity. PLoS Biol. 2011 Apr;9(4):e1001052. PubMed.
- Tatom JB, Wang DB, Dayton RD, Skalli O, Hutton ML, Dickson DW, Klein RL. Mimicking aspects of frontotemporal lobar degeneration and Lou Gehrig's disease in rats via TDP-43 overexpression. Mol Ther. 2009 Apr;17(4):607-13. PubMed.
- Wang DB, Dayton RD, Henning PP, Cain CD, Zhao LR, Schrott LM, Orchard EA, Knight DS, Klein RL. Expansive gene transfer in the rat CNS rapidly produces amyotrophic lateral sclerosis relevant sequelae when TDP-43 is overexpressed. Mol Ther. 2010 Dec;18(12):2064-74. Epub 2010 Sep 28 PubMed.
- Zhou Y, Liu S, Liu G, Oztürk A, Hicks GG. ALS-associated FUS mutations result in compromised FUS alternative splicing and autoregulation. PLoS Genet. 2013 Oct;9(10):e1003895. Epub 2013 Oct 31 PubMed.
- Polymenidou M, Lagier-Tourenne C, Hutt KR, Huelga SC, Moran J, Liang TY, Ling SC, Sun E, Wancewicz E, Mazur C, Kordasiewicz H, Sedaghat Y, Donohue JP, Shiue L, Bennett CF, Yeo GW, Cleveland DW. Long pre-mRNA depletion and RNA missplicing contribute to neuronal vulnerability from loss of TDP-43. Nat Neurosci. 2011 Apr;14(4):459-68. PubMed.
External Citations
Further Reading
Papers
- Gontijo AM, Aubert S, Roelens I, Lakowski B. Mutations in genes involved in nonsense mediated decay ameliorate the phenotype of sel-12 mutants with amber stop mutations in Caenorhabditis elegans. BMC Genet. 2009;10:14. PubMed.
- Brichta L, Garbes L, Jedrzejowska M, Grellscheid SN, Holker I, Zimmermann K, Wirth B. Nonsense-mediated messenger RNA decay of survival motor neuron 1 causes spinal muscular atrophy. Hum Genet. 2008 Mar;123(2):141-53. PubMed.
News
- San Diego: TDP-43 Targets Loom Large—But Where’s the Bull’s Eye?
- CLIPs of TDP-43 Provide a Glimpse Into Pathology
- Friends of FUS: Protein's Many RNA Buddies Point to Disease
- TDP-43 Turns Itself Off, Inclusions a False Lead
- No FUS, No ALS: Gain of Toxic Function Likely MO of Mutations
- Does ALS Gene Police RNA, Keep Strands From Entangling?
Primary Papers
- Barmada SJ, Ju S, Arjun A, Batarse A, Archbold HC, Peisach D, Li X, Zhang Y, Tank EM, Qiu H, Huang EJ, Ringe D, Petsko GA, Finkbeiner S. Amelioration of toxicity in neuronal models of amyotrophic lateral sclerosis by hUPF1. Proc Natl Acad Sci U S A. 2015 Jun 23;112(25):7821-6. Epub 2015 Jun 8 PubMed.
- Jackson KL, Dayton RD, Orchard EA, Ju S, Ringe D, Petsko GA, Maquat LE, Klein RL. Preservation of forelimb function by UPF1 gene therapy in a rat model of TDP-43-induced motor paralysis. Gene Ther. 2015 Jan;22(1):20-8. Epub 2014 Nov 6 PubMed.
Annotate
To make an annotation you must Login or Register.

Comments
Barmada et al. demonstrate that enhancing the non-sense mediated decay pathway rescues toxicity seen by the overexpression of TDP-43 and FUS. This rescue of toxicity is likely through a direct mechanism by which the auto-regulation of TDP-43 and FUS by non-sense mediated decay is enhanced. It would be interesting to know if there are any secondary benefits of UPF1 overexpression by mutating the necessary sequences for autoregulation of either TDP-43 or FUS.
Jackson et al. show that this rescue also occurs in vivo by demonstrating that UPF1 overexpression rescues both viability and phenotypic toxicities seen in a rat model of TDP-43. This suggests that the upregulation of UPF1 or the non-sense mediated decay pathway may be a potential therapeutic strategy in treating ALS patients.
We believe that UPF1 does, in fact, have beneficial effects on neuronal survival that are independent of TDP43 and/or FUS autoregulation. This is difficult to study by removing the functional autoregulatory sequences from TDP43 or FUS because we would have to alter the endogenous loci in addition to the exogenous cDNA. We are nonetheless attempting to answer this question through global approaches.
We were excited to see the effects of UPF1 in vivo as determined by Jackson et al., and look forward to adapting UPF1 and/or other modifiers of RNA decay into valid therapeutics.
In our paper (Jackson et al., 2015), we measured endogenous levels of TDP-43 mRNA to address auto-regulation. We also carefully studied whether co-expressing two transgenes with AAV resulted in non-specific gene competition. The data in the paper support that neither issue played a role in the beneficial behavioral outcome.
References:
Jackson KL, Dayton RD, Orchard EA, Ju S, Ringe D, Petsko GA, Maquat LE, Klein RL. Preservation of forelimb function by UPF1 gene therapy in a rat model of TDP-43-induced motor paralysis. Gene Ther. 2015 Jan;22(1):20-8. Epub 2014 Nov 6 PubMed.
Make a Comment
To make a comment you must login or register.