Enter the New Alzheimer’s Gene: TREM2 Variant Triples Risk
Quick Links
Rare mutations in a microglial receptor contribute as much to Alzheimer’s risk as does the more common ApoE4 genotype, according to back-to-back papers in the November 14 New England Journal of Medicine online. Variants in the triggering receptor expressed on myeloid cells 2 (TREM2) approximately triple one’s risk of developing AD, both sets of authors report. In the brain, TREM2 seems important for microglial signaling. “It firmly puts the microglial response center stage,” said John Hardy of University College London, U.K. Hardy led The Alzheimer Genetic Analysis Group that conducted one of the studies. The other comes from deCODE Genetics in Reykjavik, Iceland, which has mined that country’s genealogical records and genomes to discover genes linked to disease. This study represents the second big Alzheimer’s find for deCODE this year: They also reported, in July, a protective amyloid precursor protein variant (see ARF related news story on Jonsson et al., 2012).
TREM2 straddles the membrane of many immune cell types, including macrophages, dendritic cells, osteoclasts, and microglia (the last two are the resident immune cells of bone and brain, respectively). Researchers know little about its ligands, but have determined that it partners with the adapter protein DAP12 (DNAX activating protein of 12 kilodaltons) to drive downstream signaling. Its few known roles include regulating inflammation and phagocytosis (Takahashi et al., 2005; Hamerman et al., 2006).
Homozygous mutations in either TREM2 or DAP12 result in Nasu-Hakola disease, which manifests as a combination of bone cysts and dementia (Paloneva et al., 2002). Recently, Hardy and colleagues discovered that some of the same TREM2 homozygous mutations produce frontotemporal dementia without the bone disease (see ARF related news story on Guerreiro et al., 2012). Now, they report that carrying a just a single TREM2 mutation predisposes one to AD as well.
All Signs Point to TREM2
The FTD finding led Hardy and colleagues to look for TREM2 variants in other genome and exome sequences the geneticists have collected, in case the mutations might show up in Alzheimer’s. They also asked collaborators Alison Goate and Carlos Cruchaga at Washington University in St. Louis, Missouri, to check their collection. Between the two groups, the scientists examined 1,092 sequences from people with AD and 1,107 from control cases. People with Alzheimer’s were particularly likely to carry one of several rare TREM2 variants. An arginine-to-histidine substitution at amino acid 47 (R47H) led the pack with the strongest association with AD; other variants were even rarer and thus harder to link to disease, Hardy told Alzforum.
To confirm the AD association, the researchers checked a meta-analysis of three genomewide association studies. Again, R47H showed up more often in cases than controls. Finally, Rosa Rademakers and collaborators at the Mayo Clinic in Jacksonville, Florida, genotyped the R47 locus in a further 1,134 AD cases and 2,834 controls, clinching the relationship between the mutation and disease.
The deCODE team, led by first author Thorlakur Jonsson and senior author Kari Stefansson, came upon the same mutation by slightly different methods. deCODE has sequenced the genomes of 2,261 Icelanders, and developed a list of variants likely to interfere with protein function. They can then examine these variants in different populations to find genes that affect complex phenotypes.
At the start, Stefansson and colleagues were not looking specifically for Alzheimer’s risk genes, but for variants that affect when people require nursing home care, he told Alzforum. They compared genetic markers in people who moved into a home by the age of 75 to those in folks still independent at 85. The R47H substitution in TREM2 appeared to influence the chances a person would enter a nursing home. Looking more closely at 3,550 people with AD and 1,236 elderly controls, the researchers determined that Alzheimer’s explained the nursing home pattern. They also found that elderly carriers of the TREM2 variant who did not exhibit AD nonetheless performed worse in cognitive tests than non-carriers. The deCODE group also genotyped separate sample sets from the United States, Germany, and the Netherlands to confirm the association with AD. In Iceland, the R47H variant appeared at a frequency of 0.63 percent, deCODE reported. "The variant is much more common than those found in APP and presenilin, and it is much rarer than ApoE4, but it has an effect size the same as ApoE4 or perhaps a bit stronger," said Hardy.
Lars Bertram of the Max-Planck Institute for Molecular Genetics in Berlin, Germany, was pleased to see that the advanced genetic technology applied by the groups yielded results. However, he confessed he was underwhelmed at the impact of TREM2 on the general population. Many risk factors in the AlzGene database explain more cases, he noted. Because the variant is so rare, he said, it is difficult to estimate its effect. Its influence on Alzheimer’s risk may be lower than that calculated in the papers, Bertram speculated.
Mechanism Points to Microglia
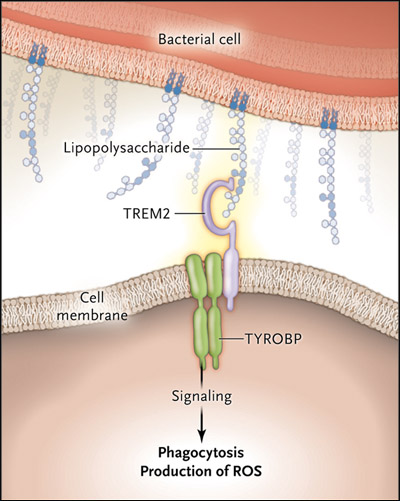
Despite their rarity, the TREM2 variants offer clues about AD pathology. “This finding points a big red arrow at microglia,” said Richard Ransohoff of the Cleveland Clinic in Ohio, who was not involved in either study (see image below). Just like the discovery of amyloid precursor protein mutations shored up the amyloid hypothesis, the TREM2 mutations support a role for neuroinflammation in Alzheimer’s. “It is the strongest evidence we have that inflammation is integral to the AD disease process,” Ransohoff said. Hardy hypothesized that TREM2 dampens microglial activation, and that the mutation results in runaway inflammation. He added that TREM2 mutations probably do not directly cause Alzheimer’s, but instead result in a state in which the brain cannot effectively combat the pathology initiated by some other cause.
The microglial receptor TREM2 is now linked to Alzheimer's disease. One of its functions is to activate phagocytosis, shown here in response to the lipopolysaccharide on a bacterial invader. Image courtesy of New England Journal of Medicine © 2012
Hardy’s idea is one among many possibilities. The AD link could also have to do with the receptor’s role in promoting microglial survival, suggested Marco Colonna of Washington University in St. Louis, Missouri. Colonna was not involved in the studies but originally cloned the TREM2 gene (Bouchon et al., 2000). In mice, he has found that loss of either TREM2 or DAP12 results in the disappearance of microglia as the animals age (Otero et al., 2009). “My suspicion would be that people who are heterozygous for the TREM2 variant will probably have defective microglia function or survival, and that will ultimately result in increased susceptibility to neurodegeneration,” he said.
Or might it be that TREM2 affects AD pathology via phagocytosis? Microglia swallow debris and apoptotic cells, and participate in synapse remodeling (see ARF related news story on Tremblay et al., 2010). The mutations might contribute to disease by inappropriately promoting or blocking the phagocytosis of synapses, speculated Mariko Bennett of Stanford University in Palo Alto, California. “One possibility is that this mutation unleashes the cells to the extent that they will attack normal tissue as well as debris,” Stefansson added.
Microglia also gobble up amyloid (Lee and Landreth, 2010), and TREM2-expressing microglia hover at the edges of plaques in AD model mice (Frank et al., 2008). That might hint that TREM2-deficient microglia in R47H carriers might fail to clean up amyloid. The authors of an editorial accompanying the Journal papers disagree. Because people with Nasu-Hakola disease do not develop amyloid plaques, TREM2 mutations probably do not affect amyloid clearance, wrote Harald Neumann of the University of Bonn, Germany, and Mark Daly of Massachusetts General Hospital in Boston.
TREM2 is so poorly understood that it is too early to say how it might contribute to disease, Ransohoff said.
TREM2 agonists might make a good therapeutic, Hardy and Stefansson agreed, by ramping up the activity of the normal TREM2 protein present in heterozygotes. Medicines that modulate inflammation also hold promise, Ransohoff said.
As they continue to sift genotypes, researchers will likely find more rare variants with strong effects, Ransohoff predicted. DAP12, TREM2’s partner, would be a good place to look, Colonna suggested. Both Hardy and Stefansson have checked DAP12, with no hits thus far.—Amber Dance
References
News Citations
- Protective APP Mutation Found—Supports Amyloid Hypothesis
- Mutations in TREM2 Cause Frontotemporal Dementia
- No Rest for Microglia: These Immune Cells Manage Healthy Synapses
Paper Citations
- Jonsson T, Atwal JK, Steinberg S, Snaedal J, Jonsson PV, Bjornsson S, Stefansson H, Sulem P, Gudbjartsson D, Maloney J, Hoyte K, Gustafson A, Liu Y, Lu Y, Bhangale T, Graham RR, Huttenlocher J, Bjornsdottir G, Andreassen OA, Jönsson EG, Palotie A, Behrens TW, Magnusson OT, Kong A, Thorsteinsdottir U, Watts RJ, Stefansson K. A mutation in APP protects against Alzheimer's disease and age-related cognitive decline. Nature. 2012 Aug 2;488(7409):96-9. PubMed.
- Takahashi K, Rochford CD, Neumann H. Clearance of apoptotic neurons without inflammation by microglial triggering receptor expressed on myeloid cells-2. J Exp Med. 2005 Feb 21;201(4):647-57. PubMed.
- Hamerman JA, Jarjoura JR, Humphrey MB, Nakamura MC, Seaman WE, Lanier LL. Cutting edge: inhibition of TLR and FcR responses in macrophages by triggering receptor expressed on myeloid cells (TREM)-2 and DAP12. J Immunol. 2006 Aug 15;177(4):2051-5. PubMed.
- Paloneva J, Manninen T, Christman G, Hovanes K, Mandelin J, Adolfsson R, Bianchin M, Bird T, Miranda R, Salmaggi A, Tranebjaerg L, Konttinen Y, Peltonen L. Mutations in two genes encoding different subunits of a receptor signaling complex result in an identical disease phenotype. Am J Hum Genet. 2002 Sep;71(3):656-62. Epub 2002 Jun 21 PubMed.
- Bouchon A, Dietrich J, Colonna M. Cutting edge: inflammatory responses can be triggered by TREM-1, a novel receptor expressed on neutrophils and monocytes. J Immunol. 2000 May 15;164(10):4991-5. PubMed.
- Otero K, Turnbull IR, Poliani PL, Vermi W, Cerutti E, Aoshi T, Tassi I, Takai T, Stanley SL, Miller M, Shaw AS, Colonna M. Macrophage colony-stimulating factor induces the proliferation and survival of macrophages via a pathway involving DAP12 and beta-catenin. Nat Immunol. 2009 Jul;10(7):734-43. PubMed.
- Tremblay MÈ, Lowery RL, Majewska AK. Microglial interactions with synapses are modulated by visual experience. PLoS Biol. 2010;8(11):e1000527. PubMed.
- Lee CY, Landreth GE. The role of microglia in amyloid clearance from the AD brain. J Neural Transm. 2010 Aug;117(8):949-60. PubMed.
- Frank S, Burbach GJ, Bonin M, Walter M, Streit W, Bechmann I, Deller T. TREM2 is upregulated in amyloid plaque-associated microglia in aged APP23 transgenic mice. Glia. 2008 Oct;56(13):1438-47. PubMed.
Other Citations
External Citations
Further Reading
Papers
- Kaneko M, Sano K, Nakayama J, Amano N. Nasu-Hakola disease: The first case reported by Nasu and review. Neuropathology. 2010 May 24; PubMed.
- Numasawa Y, Yamaura C, Ishihara S, Shintani S, Yamazaki M, Tabunoki H, Satoh JI. Nasu-Hakola disease with a splicing mutation of TREM2 in a Japanese family. Eur J Neurol. 2011 Sep;18(9):1179-83. PubMed.
- Bajramovic JJ. Regulation of innate immune responses in the central nervous system. CNS Neurol Disord Drug Targets. 2011 Feb 1;10(1):4-24. PubMed.
- Linnartz B, Wang Y, Neumann H. Microglial immunoreceptor tyrosine-based activation and inhibition motif signaling in neuroinflammation. Int J Alzheimers Dis. 2010;2010 PubMed.
- Melchior B, Garcia AE, Hsiung BK, Lo KM, Doose JM, Thrash JC, Stalder AK, Staufenbiel M, Neumann H, Carson MJ. Dual induction of TREM2 and tolerance-related transcript, Tmem176b, in amyloid transgenic mice: implications for vaccine-based therapies for Alzheimer's disease. ASN Neuro. 2010 Jul 12;2(3):e00037. PubMed.
- Frank S, Burbach GJ, Bonin M, Walter M, Streit W, Bechmann I, Deller T. TREM2 is upregulated in amyloid plaque-associated microglia in aged APP23 transgenic mice. Glia. 2008 Oct;56(13):1438-47. PubMed.
News
- Mutations in Microglia Protein Cause Rare Dementia
- Australia Report: Inflammation
- Call in BACE1 Inhibitors for Nerve Repair Duty?
- Barcelona: Inflammation—That Two-Faced Beast
- Immune Phosphatase Underlies Microglia’s Split Personality in AD
- New Pathways With Promise in AD—An Inflammatory Statement?
- Protective APP Mutation Found—Supports Amyloid Hypothesis
- Mutations in TREM2 Cause Frontotemporal Dementia
- No Rest for Microglia: These Immune Cells Manage Healthy Synapses
Primary Papers
- Guerreiro R, Wojtas A, Bras J, Carrasquillo M, Rogaeva E, Majounie E, Cruchaga C, Sassi C, Kauwe JS, Younkin S, Hazrati L, Collinge J, Pocock J, Lashley T, Williams J, Lambert JC, Amouyel P, Goate A, Rademakers R, Morgan K, Powell J, St George-Hyslop P, Singleton A, Hardy J, Alzheimer Genetic Analysis Group. TREM2 variants in Alzheimer's disease. N Engl J Med. 2013 Jan 10;368(2):117-27. Epub 2012 Nov 14 PubMed.
- Neumann H, Daly MJ. Variant TREM2 as risk factor for Alzheimer's disease. N Engl J Med. 2013 Jan 10;368(2):182-4. PubMed.
- Jonsson T, Stefansson H, Steinberg S, Jonsdottir I, Jonsson PV, Snaedal J, Bjornsson S, Huttenlocher J, Levey AI, Lah JJ, Rujescu D, Hampel H, Giegling I, Andreassen OA, Engedal K, Ulstein I, Djurovic S, Ibrahim-Verbaas C, Hofman A, Ikram MA, van Duijn CM, Thorsteinsdottir U, Kong A, Stefansson K. Variant of TREM2 associated with the risk of Alzheimer's disease. N Engl J Med. 2013 Jan 10;368(2):107-16. Epub 2012 Nov 14 PubMed.
Annotate
To make an annotation you must Login or Register.

Comments
Klinik und Poliklinik für Neurologie
Triggering receptor expressed on myeloid cells 2 (TREM2) represents a surface receptor without its own intracellular signaling motif. It therefore depends on the adaptor protein 12 (DAP12) for the initiation of signaling cascades. TREM2 has been primarily found and investigated in myeloid cells, and thus far, TREM2 and DAP12 mutations have only been known to be involved in progressive presenile dementia in patients suffering from polycystic lipomembranous osteodysplasia with sclerosing leukoencephalopathy (Nasu-Hakola disease), a rare autosomal recessive disorder.
The reports from Jonsson et al. and Guerreiro et al. now convincingly suggest that rare, heterozygous variants of the TREM2 gene, which most likely result in a reduced function of this receptor, are pathogenetically involved in sporadic AD. In the human cerebral cortex, TREM2 expression has been described in microglia and, to a smaller extent, in neurons (Sessa et al., 2004). Importantly, TREM2 has been described to be expressed by non-activated microglia (Schmid et al., 2002), but also can be found at the border of amyloid-β (Aβ) plaque deposits in APP transgenic mice (Frank et al., 2008), thus implicating TREM2 in the innate immune response to Aβ accumulation and deposition in the brain.
Innate immune activation and neurodegenerative pathways interact at multiple levels, and this mutual interaction may ultimately function as an important motor of neurodegeneration (for a review see, e.g., (Lucin and Wyss-Coray, 2009; Heneka and O’Banion, 2007). Given the pro-phagocytic and anti-inflammatory role of TREM2 (Takahashi et al., 2005), expression of TREM2 by Aβ plaque-associated microglia may be interpreted as an effort to support Aβ clearance and to limit the proinflammatory cytokine expression in response to microglia activation by Aβ itself.
Knockdown of TREM2 in microglia increased the gene transcription of nitric oxide (NO) synthase 2 (NOS2) and tumor necrosis factor α (TNF-α) (Takahashi et al., 2005). As NOS2-derived NO may directly enhance Aβ aggregation (Kummer et al., 2011), and acts in concert with TNF-α to suppress hippocampal long-term potentiation (Wang et al., 2004; Wang et al., 2005), loss-of-function mutations in TREM2 may promote AD neuroinflammation and thereby drive neuronal degeneration. Likewise, TREM2 expression has been positively correlated with the phagocytic clearance of Aβ in APP transgenic mice (Melchior et al., 2010). Since impaired Aβ clearance has been suggested as the underlying cause of sporadic AD (Mawuenyega et al., 2010), loss of phagocytic efficacy due to TREM2 mutations could represent a possible mechanism by which the described mutations increase the risk to develop AD.
Further support for TREM2 being an important mediator in neuroinflammation comes from multiple sclerosis (MS), where soluble TREM2 has been found to be increased in patients suffering from relapsing-remitting and primary progressive MS (Piccio et al., 2008). Intriguingly, inhibition of TREM2 function potentiated pathology in the related murine model of experimental autoimmune encephalomyelitis (Piccio et al., 2007).
References:
Sessa G, Podini P, Mariani M, Meroni A, Spreafico R, Sinigaglia F, Colonna M, Panina P, Meldolesi J. Distribution and signaling of TREM2/DAP12, the receptor system mutated in human polycystic lipomembraneous osteodysplasia with sclerosing leukoencephalopathy dementia. Eur J Neurosci. 2004 Nov;20(10):2617-28. PubMed.
Schmid CD, Sautkulis LN, Danielson PE, Cooper J, Hasel KW, Hilbush BS, Sutcliffe JG, Carson MJ. Heterogeneous expression of the triggering receptor expressed on myeloid cells-2 on adult murine microglia. J Neurochem. 2002 Dec;83(6):1309-20. PubMed.
Frank S, Burbach GJ, Bonin M, Walter M, Streit W, Bechmann I, Deller T. TREM2 is upregulated in amyloid plaque-associated microglia in aged APP23 transgenic mice. Glia. 2008 Oct;56(13):1438-47. PubMed.
Lucin KM, Wyss-Coray T. Immune activation in brain aging and neurodegeneration: too much or too little?. Neuron. 2009 Oct 15;64(1):110-22. PubMed.
Heneka MT, O'Banion MK. Inflammatory processes in Alzheimer's disease. J Neuroimmunol. 2007 Mar;184(1-2):69-91. PubMed.
Takahashi K, Rochford CD, Neumann H. Clearance of apoptotic neurons without inflammation by microglial triggering receptor expressed on myeloid cells-2. J Exp Med. 2005 Feb 21;201(4):647-57. PubMed.
Kummer MP, Hermes M, Delekarte A, Hammerschmidt T, Kumar S, Terwel D, Walter J, Pape HC, König S, Roeber S, Jessen F, Klockgether T, Korte M, Heneka MT. Nitration of tyrosine 10 critically enhances amyloid β aggregation and plaque formation. Neuron. 2011 Sep 8;71(5):833-44. PubMed.
Wang Q, Rowan MJ, Anwyl R. Beta-amyloid-mediated inhibition of NMDA receptor-dependent long-term potentiation induction involves activation of microglia and stimulation of inducible nitric oxide synthase and superoxide. J Neurosci. 2004 Jul 7;24(27):6049-56. PubMed.
Wang Q, Wu J, Rowan MJ, Anwyl R. Beta-amyloid inhibition of long-term potentiation is mediated via tumor necrosis factor. Eur J Neurosci. 2005 Dec;22(11):2827-32. PubMed.
Melchior B, Garcia AE, Hsiung BK, Lo KM, Doose JM, Thrash JC, Stalder AK, Staufenbiel M, Neumann H, Carson MJ. Dual induction of TREM2 and tolerance-related transcript, Tmem176b, in amyloid transgenic mice: implications for vaccine-based therapies for Alzheimer's disease. ASN Neuro. 2010 Jul 12;2(3):e00037. PubMed.
Mawuenyega KG, Sigurdson W, Ovod V, Munsell L, Kasten T, Morris JC, Yarasheski KE, Bateman RJ. Decreased clearance of CNS beta-amyloid in Alzheimer's disease. Science. 2010 Dec 24;330(6012):1774. PubMed.
Piccio L, Buonsanti C, Cella M, Tassi I, Schmidt RE, Fenoglio C, Rinker J 2nd, Naismith RT, Panina-Bordignon P, Passini N, Galimberti D, Scarpini E, Colonna M, Cross AH. Identification of soluble TREM-2 in the cerebrospinal fluid and its association with multiple sclerosis and CNS inflammation. Brain. 2008 Nov;131(Pt 11):3081-91. Epub 2008 Sep 12 PubMed.
Piccio L, Buonsanti C, Mariani M, Cella M, Gilfillan S, Cross AH, Colonna M, Panina-Bordignon P. Blockade of TREM-2 exacerbates experimental autoimmune encephalomyelitis. Eur J Immunol. 2007 May;37(5):1290-301. PubMed.
University of Southern California
The present work can be viewed as key support for the neuroinflammation hypothesis of Alzheimer’s disease. In my mind, at least, it dovetails well with earlier work demonstrating genomewide association between another microglial proinflammatory gene, complement receptor 1, and Alzheimer’s disease (Lambert et al., 2009). Together, these and other studies mark a turning of the tide in how we fundamentally view the disease—specifically, as an inflammatory syndrome.
In regard to the present work, I find it interesting that TREM2 expression was increased in the TgCRND8 mouse model of cerebral amyloidosis. One logical follow-on question is whether interrupting TREM2 function will impact disease progression in rodent models. Given that TREM2 plays a role in mediating proinflammatory innate immune signaling by microglia, as Michael Heneka nicely pointed out, one could hypothesize that blunting neuroinflammation by knocking out TREM2 would mitigate AD-like pathology in transgenic mice. By corollary, this would suggest that blocking TREM2-mediated neuroinflammation, as opposed to promoting it, would be the therapeutic approach here.
References:
Lambert JC, Heath S, Even G, Campion D, Sleegers K, Hiltunen M, Combarros O, Zelenika D, Bullido MJ, Tavernier B, Letenneur L, Bettens K, Berr C, Pasquier F, Fiévet N, Barberger-Gateau P, Engelborghs S, De Deyn P, Mateo I, Franck A, Helisalmi S, Porcellini E, Hanon O, , de Pancorbo MM, Lendon C, Dufouil C, Jaillard C, Leveillard T, Alvarez V, Bosco P, Mancuso M, Panza F, Nacmias B, Bossù P, Piccardi P, Annoni G, Seripa D, Galimberti D, Hannequin D, Licastro F, Soininen H, Ritchie K, Blanché H, Dartigues JF, Tzourio C, Gut I, Van Broeckhoven C, Alpérovitch A, Lathrop M, Amouyel P. Genome-wide association study identifies variants at CLU and CR1 associated with Alzheimer's disease. Nat Genet. 2009 Oct;41(10):1094-9. PubMed.
University of Antwerp
These studies provide further evidence that the genetic architecture of Alzheimer's disease does indeed include rare variants of intermediate penetrance, analogous to our work on rare variants in the GRN (Brouwers et al., 2008) and CLU genes (Bettens et al., 2012). Moreover, these NEJM papers demonstrate the strength of techniques such as whole-exome sequencing to detect rare variants implicated in Alzheimer's disease, although it should be noted that large numbers of samples are required before there is sufficient basis to draw first conclusions. Of note, there was no evidence of association of the TREM2 variant in several individual replication cohorts, with the variant only reaching significance when pooling results.
One of the caveats when combining exome or genome sequence data from several sites, with controls and patients coming from different centers/platforms, is population stratification. Population allele frequency estimates seem to differ among countries. Nevertheless, association was also observed in one single large cohort from Iceland.
Discovery of a rare variant associated with AD, like the one described in TREM2, has a small epidemiological impact, but may have significant impact in understanding the pathomechanisms leading to AD.
References:
Brouwers N, Sleegers K, Engelborghs S, Maurer-Stroh S, Gijselinck I, van der Zee J, Pickut BA, Van den Broeck M, Mattheijssens M, Peeters K, Schymkowitz J, Rousseau F, Martin JJ, Cruts M, De Deyn PP, Van Broeckhoven C. Genetic variability in progranulin contributes to risk for clinically diagnosed Alzheimer disease. Neurology. 2008 Aug 26;71(9):656-64. PubMed.
Bettens K, Brouwers N, Engelborghs S, Lambert JC, Rogaeva E, Vandenberghe R, Le Bastard N, Pasquier F, Vermeulen S, Van Dongen J, Mattheijssens M, Peeters K, Mayeux R, St George-Hyslop P, Amouyel P, De Deyn PP, Sleegers K, Van Broeckhoven C. Both common variations and rare non-synonymous substitutions and small insertion/deletions in CLU are associated with increased Alzheimer risk. Mol Neurodegener. 2012;7:3. PubMed.
Case Western Reserve University
With the increasing acceptance (1) that Alzheimer’s disease is a multifactorial disorder (2), it might be a mistake to interpret every new finding on Alzheimer’s disease through the amyloid lens (see Michael Heneka’s comment above). As Neumann and Daly pointed out in their NEJM commentary, amyloid plaques have not been reported in Nasu-Hakola patients despite a near-complete loss of function of TREM2 and progressive presenile inflammatory neurodegeneration. Thus, increased AD risk in TREM2 variants is just as likely to be independent of amyloid, and future investigations should be designed/interpreted accordingly.
Looking back, we could argue that a similar mistake was made when epidemiological data on NSAIDs’ protective effects against developing AD were interpreted in terms of NSAIDs' ability to inhibit γ-secretase cleavage (3). This resulted in subsequent confusing data on various NSAIDs and Aβ production, and perhaps muddied NSAIDs' potential as therapeutic drugs. Perhaps we need to ponder whether our inability to think outside the amyloid framework is inhibiting the field from making faster progress towards an effective therapeutic treatment.
References:
Storandt M, Head D, Fagan AM, Holtzman DM, Morris JC. Toward a multifactorial model of Alzheimer disease. Neurobiol Aging. 2012 Oct;33(10):2262-71. PubMed.
Pimplikar SW. Reassessing the amyloid cascade hypothesis of Alzheimer's disease. Int J Biochem Cell Biol. 2009 Jun;41(6):1261-8. PubMed.
Weggen S, Eriksen JL, Das P, Sagi SA, Wang R, Pietrzik CU, Findlay KA, Smith TE, Murphy MP, Bulter T, Kang DE, Marquez-Sterling N, Golde TE, Koo EH. A subset of NSAIDs lower amyloidogenic Abeta42 independently of cyclooxygenase activity. Nature. 2001 Nov 8;414(6860):212-6. PubMed.
Make a Comment
To make a comment you must login or register.