A Blood Test for Preclinical Prion Disease, But Will It Be Used?
Quick Links
Researchers can now detect misfolded prion proteins in the blood of humans and primates in the asymptomatic stages of variant Creutzfeldt-Jakob Disease (vCJD). Thousands of people were exposed to this prion disease by eating meat from cattle with bovine spongiform encephalitis (BSE); however, how many people truly carry the bad seeds in their blood is unknown. This week’s recall of beef distributed to the U.S. chain Whole Foods because it contained nervous-system tissue is a reminder of continued concern of a potential threat from vCJD. Writing in the June 12 PLOS Pathogens, researchers led by Olivier Andréoletti at the National Veterinary School of Toulouse, France, report a technique to detect tiny amounts of toxic prions in blood. The researchers hope such a test will be used to determine the prevalence of latent vCJD in the European population, especially in the United Kingdom, where exposure to the disease was highest. Such a test could also prove useful for screening donor blood prior to transfusion, but a lack of political will prevents it from moving forward, according to Andréoletti and other researchers.
The study provides the first evidence that vCJD can be detected in asymptomatic primates, which most closely model the human forms of the disease, Andréoletti wrote in an email to Alzforum. The results suggest that asymptomatic human carriers may also be detected with the test.
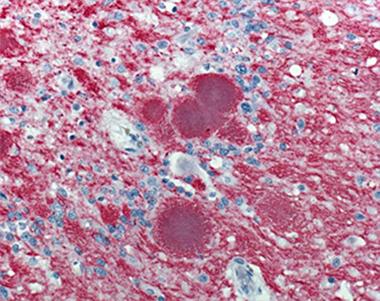
A cerebellar sample from a patient who died of vCJD.
In the late ’80s and early ’90s, thousands of people in the U.K. were exposed to BSE, better known as mad cow disease. The exposure resulted in 225 confirmed cases of prion disease that then became known as variant CJD. CJD is a fatal neurodegenerative disease mediated by misfolding of the normally innocuous prion protein. Despite the small number of confirmed vCJD cases, recent evidence emerged from the histological examination of appendix samples suggesting that one in 2,000 people in the U.K. harbored the potentially lethal prions (see Gill et al., 2013). The possibility of thousands of asymptomatic carriers of potentially infectious vCJD has led to concerns about transfer of the prion through blood transfusion. Four documented cases of likely transmission from vCDJ-carrying blood donors to recipients have been documented so far (see Llewelyn et al., 2004; Peden et al., 2004).
Efforts to develop reliable blood tests for asymptomatic vCJD have been underway for more than a decade. In one method—protein misfolding cyclic amplification (PMCA)—researchers amplify small amounts of misfolded prion proteins within a sample by using them as seeds to corrupt normally folded prion protein. After repeated rounds of sonication to split up newly formed seeds, investigators can detect what was once a minute amount of toxic prion protein. First developed by Claudio Soto at the University of Texas in Houston, this assay detected prions in the blood and urine of animals (see Castilla et al., 2005; Saa et al., 2006; and Gonzales-Romero et al., 2008). Whether it can pick up toxic prions in human blood has not been shown, as most of the precious few samples from vCJD-infected people are carefully guarded by a tissue bank in the U.K., Andréoletti told Alzforum. Soto’s lab is in the process of completing the required validation procedures—which involve screening vCJD-spiked blood samples as well as thousands of healthy blood samples from unaffected countries—to gain access to the vCJD blood samples, but Andréoletti said the requirements were too costly for his lab.
Andréoletti’s lab optimized the PMCA assay in blood of various animals, including asymptomatic primates, and also tried out the assay in four available human samples. First author Caroline Lacroux and colleagues started by screening for the best source of normal prion protein to tempt toxic seeds into amplification. To that end, the researchers extracted protein from the brains of transgenic mice expressing normal forms of human, cow, or sheep PrP. The researchers then seeded these substrates with toxic forms of prions extracted from postmortem brain samples of BSE-infected animals or a vCJD-infected person. To Andréoletti’s surprise, the sheep PrP proved to be the most efficient substrate at amplifying toxic prions from all species.
After confirming that the sheep substrate could be used to detect toxic prion protein in the blood of sheep that were presymptomatic for scrapie, Lacroux and colleagues used the assay to see how early they could detect toxic prions in the blood of primates infected with vCJD. They detected the corrupted prion protein in blood from monkeys as early as 10 months after infection—about 32 months prior to the onset of vCJD symptoms.
The researchers next tested their assay on blood from the four confirmed vCJD patients—one from the Hospital of Lyon in France, and three others from the Medical Research Council in London—along with 135 healthy controls from France and nine controls from the MRC. Three out of the four vCJD blood samples tested positive for the disease; none of the controls did.
While these results suggest the test could avoid the dreaded caveat of false-positive results, Soto thinks the small number of samples precludes conclusions. “They did the best they could with the number of human samples available,” he said. “What makes this paper interesting are the results from asymptomatic primates. They show that you can detect vCJD in the blood early on.”
For his part, Soto is testing the validity of the PMCA test in urine samples from vCJD patients, which are more widely available, he said. Even though his test remains untried in human blood, Soto thinks it could be useful as a screening tool. “The technology clearly works if you know how to use it,” he said. “This is the way to go for testing. The question is: Will it be done or not?”
The small number of documented vCJD cases has created a false sense of security about the danger of the disease, Soto claims, and that has hampered efforts to test the population or blood products. However, he said that the disease’s long incubation period could mean that the threat is greater than most realize.
Soto has turned his efforts to developing the PMCA test to detect early onset of Alzheimer’s disease. Having used the test to measure seed-like Aβ oligomers in cerebrospinal fluid (see Mar 2014 news story), he is now testing it in blood. Andréoletti’s lab is also working on using seed-based assays to detect AD.
“PMCA and other newly developed techniques … open a completely new field for detection of misfolded proteins,” Inga Zerr of Georg-August University in Gottingen, Germany, wrote in an email to Alzforum. “This might be relevant not only for prion diseases of humans and animals, but also other degenerative disorders such as Alzheimer’s disease or synucleinopathies.” (See full comment below.)—Jessica Shugart
References
News Citations
Paper Citations
- Gill ON, Spencer Y, Richard-Loendt A, Kelly C, Dabaghian R, Boyes L, Linehan J, Simmons M, Webb P, Bellerby P, Andrews N, Hilton DA, Ironside JW, Beck J, Poulter M, Mead S, Brandner S. Prevalent abnormal prion protein in human appendixes after bovine spongiform encephalopathy epizootic: large scale survey. BMJ. 2013 Oct 15;347:f5675. PubMed.
- Llewelyn CA, Hewitt PE, Knight RS, Amar K, Cousens S, Mackenzie J, Will RG. Possible transmission of variant Creutzfeldt-Jakob disease by blood transfusion. Lancet. 2004 Feb 7;363(9407):417-21. PubMed.
- Peden AH, Head MW, Ritchie DL, Bell JE, Ironside JW. Preclinical vCJD after blood transfusion in a PRNP codon 129 heterozygous patient. Lancet. 2004 Aug 7-13;364(9433):527-9. PubMed.
- Castilla J, Saá P, Soto C. Detection of prions in blood. Nat Med. 2005 Sep;11(9):982-5. PubMed.
- Saá P, Castilla J, Soto C. Presymptomatic detection of prions in blood. Science. 2006 Jul 7;313(5783):92-4. PubMed.
- Gonzalez-Romero D, Barria MA, Leon P, Morales R, Soto C. Detection of infectious prions in urine. FEBS Lett. 2008 Sep 22;582(21-22):3161-6. Epub 2008 Aug 13 PubMed.
External Citations
Further Reading
No Available Further Reading
Primary Papers
- Lacroux C, Comoy E, Moudjou M, Perret-Liaudet A, Lugan S, Litaise C, Simmons H, Jas-Duval C, Lantier I, Béringue V, Groschup M, Fichet G, Costes P, Streichenberger N, Lantier F, Deslys JP, Vilette D, Andréoletti O. Preclinical detection of variant CJD and BSE prions in blood. PLoS Pathog. 2014 Jun;10(6):e1004202. Epub 2014 Jun 12 PubMed.
Annotate
To make an annotation you must Login or Register.

Comments
�
Risk of blood-born transmission of variant CJD has been a matter of concern for many years. Strong measures such as blood filtration and donor exclusion criteria have been adapted in order to minimize the risk for humans. Only few blood transfusion-related cases have been identified so far, however, a recent study in the U.K. reported the presence of PK-resistant PrP in asymptomatic carriers in appendices and estimated the prevalence of vCJD in the general population as high as 1:2000 in the age cohort born between 1941 and 1985.
These high numbers are in contrast to few clinically affected patients on one hand, and only few cases which could be linked to blood transfusions on the other. However, in the absence of a definite screening test, the potential for disease transmission between humans via blood remains.
The work reported here relates to the further development of the protein amplification technique, which was reported for the first time by Claudio Soto (Soto et al., 2002) and is called PMCA-protein misfolding cyclic amplification. The basic principle is the amplification of misfolded prion aggregates via repeated sonication and seeding with various substrates, which lead to detectable levels of the abnormal protein.
PMCA has been demonstrated to work in various fluids and now, for the first time, using blood of affected patients. In addition, the pathological aggregates were detected at early clinical and preclinical disease stages in animal models. In humans, the assay identified three out of four vCJD samples, which demonstrates the possibility for blood test development. Further methodological development on test stability and robustness as well as applicability will follow.
PMCA and other newly developed techniques, such as RT-QuIC and eQuIC, open a completely new field for detection of misfolded proteins, which might be relevant not only for prion diseases of humans and animals, but also other degenerative disorders, Alzheimer’s disease, or synucleinopathies.
References:
Soto C, Saborio GP, Anderes L. Cyclic amplification of protein misfolding: application to prion-related disorders and beyond. Trends Neurosci. 2002 Aug;25(8):390-4. PubMed.
Make a Comment
To make a comment you must login or register.