Brain Damage from Cardiovascular Disease Starts Earlier Than You Think
Quick Links
Scientists agree that midlife cardiovascular risk factors portend late-life dementia. But exactly when in midlife? Two separate, but complementary, studies presented at this year’s Alzheimer’s Association International Conference, held July 22–26 in Chicago, come down firmly in the 40s and even earlier.
Matthew Pase, Swinburne University of Technology, Hawthorn, Australia, collaborated with Charles DeCarli at University of California, Davis, to analyze data from the Framingham Heart Study. Pase reported that no matter how long a person lived, his or her risk for future brain atrophy due to cardiovascular disease had always been highest when they were about 45. “The study suggests that the effects of cardiovascular risk factors on the brain are much more robust in the 40s and then diminish as people get older,” said DeCarli.
Similarly, Christopher Lane, from University College London, England, reported that in a cohort followed from birth, high blood pressure at age 53, and rising blood pressure in the decade before that, correlated with damage to small blood vessels in the brain at about age 70. Hypertension in the 40s also correlated with later-life brain atrophy. In marked contrast, Lane found no link between blood pressure and accumulation of brain amyloid. “The relationship between midlife hypertension and vascular disease was expected. What was less clear was the epoch when that risk was strongest, that acceleration as well as absolute levels of blood pressure was important, and that the effect of blood pressure was on small vessel disease and brain volume but not amyloid accumulation,” noted Jonathan Schott, who led the UCL study.
Vascular risk factors in the 40s and 50s, including hypertension, have been linked to later-life dementia (Aug 2017 news; Jun 2018 news). Others had previously reported that the sooner in life blood pressure rises, the stronger it associates with late-life structural damage in the brain. Most of those studies have been limited to specific populations (Swan et al., 1998; Power et al., 2016; Knopman et al., 2011; Debette et al., 2011).
Schott and colleagues study a birth cohort that is representative of the whole of mainland Britain. It has been followed prospectively since 1946. At that time, the British government was concerned that population growth would be insufficient to support rebuilding the country after the decimation of World War II. They commissioned a survey of every birth in the U.K. during a single week, March 3 to 9, all 13,687 of them. Then, recognizing an opportunity to learn how the environment shapes mental and physical development, the government decided to track a representative sample of those babies, following 5,362 singletons who had been born to married parents. The National Survey of Health and Development has since seen and tested the men and women of this cohort 24 times.
In the early days, the survey took stock of educational attainment, socioeconomic status, diet, exercise, and mental health. In 1982, when the cohort were 36 years old, they began receiving more extensive clinical tests, including blood pressure measurements and tests for respiratory, cognitive, and musculoskeletal function. Between ages 60 and 64, members of the cohort were offered more intensive cardiac screening. About 1,200 accepted and underwent EKG, echocardiograms, and Doppler ultrasound of the carotid arteries to look for arterial plaques. “We know an enormous amount about these volunteers,” said Schott.
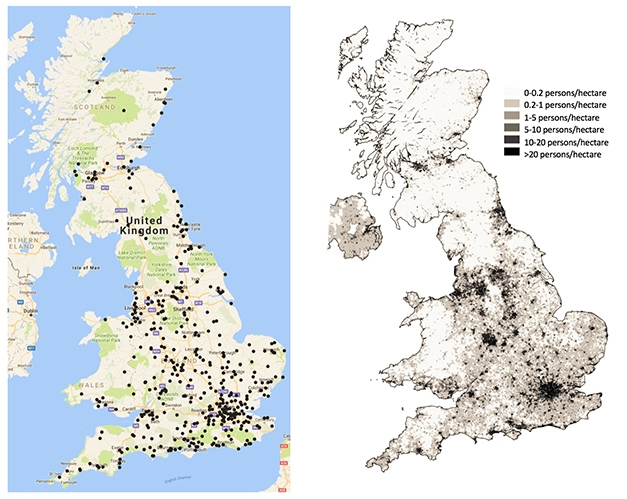
Representative Sample. Distribution of volunteers in Insight46 (black dots, left), reflect the population density of the U.K. (right). [Courtesy of Jonathan Schott.]
To learn about their brain health, Schott, together with Nick Fox and Marcus Richards at UCL, began the Insight46 study (Lane et al., 2017). This sub-study selected 500 of the people who had volunteered for more intensive cardio testing in their early 60s. It plans to scan their brains with structural MRI and florbetapir amyloid PET twice, two years apart. Baseline assessments began in 2015 and were finished in January of this year. Insight46 also collects clinical, neuropsychological, fluid biomarker, and genetic information. In his talk at AAIC, Lane focused on how the imaging data relate to blood pressure.
Lane wanted to know how three measures—brain amyloid, brain volume, and white-matter lesions reflecting damage to the brain’s teeny blood vessels—relate both to absolute blood pressure values and their rate of change. Blood pressure had been taken when the cohort was 36, 43, 53, 60–64, and 69 years old. Systolic blood pressure (SBP) steadily rose during this time from about 125mmHg to 134mmHg for men, and from about 115mmHg to 131mmHg for women. Diastolic pressure (DP) rose initially, too, from about 81mmHg to 86mmHg for men and from 76mmHg to 80mmHg for women, but began to fall at age 53 to end up at about 74mmHg for men and 73mmHg for women by age 69. How would these numbers relate to brain health?
Associations were extremely narrow. Lane reported that only at age 53 did higher SBP and DBP correlate with the extent of white-matter hyperintensities (WMHs) at 69, even though the SBP held steady from age 53–69. The change in both SBP and DBP between ages 43 and 53 correlated with WMHs as well, but the change over other decades did not. What does this mean? The idea is that having higher blood pressure during that specific decade puts people at risk for brain damage in later life.
Analysis of whole brain volume told a similar story, albeit the risk might come sooner. Lane reported that higher DBP at age 43, and the change in DBP from age 36–43, correlated with smaller brain volumes.
Lane thinks it important not only that the absolute blood pressure tracked with brain damage, but also the change in pressure. “We know high blood pressure is bad for cardiovascular and cerebrovascular health, and the benefits of screening are well recognized, but that does not take account of previous blood pressure over time,” he told Alzforum. “We should be thinking of monitoring change as well as the absolute number,” he said. This could be done with wearable devices, Lane suggested.
DeCarli said the study complemented many others in the field. “Drawn from an entire population across mainland Britain, the birth cohort confirms and extends what others have shown, namely that the effect of cardiovascular disease on brain health is stronger in midlife,” he told Alzforum.
That said, DeCarli thinks Insight46 underestimated the effect, because the MRI measurements were taken when the volunteers were in their 70s. He, Pase, and colleagues correlated cardiovascular risk with brain lesions both cross-sectionally and longitudinally in participants of the Framingham Heart Study. In 1948 the FHS began to track the cardiovascular health of some 5,000 volunteers, aged 30–59. It is now in its third iteration, having recruited children and grandchildren of the original cohort in 1971 and 2002, respectively. Volunteers began having brain MRI scans around 1999. Pase correlated brain volume measured by MRI with scores on the Framingham Stroke Risk Profile, a validated and widely used measure of overall cardiovascular risk based on a plethora of parameters including, age, gender, cardiovascular disease, atrial fibrillation, diabetes, blood pressure, and tobacco smoking history.
At AAIC, Pase reported that in cross-sectional analysis, higher stroke risk correlated with smaller brain volume at that same point in time. The association was strongest in those aged 45. Similarly, when he looked prospectively at how stroke risk relates to future brain volume, he again found the greatest threat came in the 40s, no matter how old the person became. For example, in those aged 85, brain volume more tightly correlated with stroke risk at age 45 than at age 55, 65, or 75 (see image below). The same was true for 75- and 65-year-olds—in each case the strongest risk for brain atrophy came at age 45. The effect was even stronger in women.

Midlife Crisis. On average, cardiovascular risk for late-life brain volume loss (beta estimates of effect size) is strongest at age 45, no matter when the atrophy occurs. [Courtesy of Matthew Pase.]
Schott thinks the Framingham data dovetails with his group’s discovery in the U.K. cohort. “While they used a composite of vascular risk rather than blood pressure, they showed that, the further in time from the brain volume measure, the stronger the association. They found a very similar effect,” he told Alzforum.
To Lane, this is an eye-opener. “Midlife is often thought to be from 40 onwards, but we see effects on the brain from age 36–43. We need to consider the risk of high blood pressure earlier in life,” he said. Alas, DeCarli thought that finding curious. “We have looked at 30-year-olds in the Framingham study, and find very few who have hypertension. It is much more common by age 50, when 25 percent of the population are affected,” he said. DeCarli added that people who have hypertension already in their 30s are in big trouble. “I suspect many of those people do not even survive to their 70s,” he said.
Alzheimer’s or Dementia?
Regarding amyloid, a link between midlife hypertension and plaques later in life has been harder to pin down. Some postmortem and PET studies have suggested a correlation (Petrovitch et al., 2000; Langbaum et al., 2012), but David Knopman, Mayo Clinic, Rochester, Minnesota, told Alzforum that both the Atherosclerosis Risk in Communities (ARIC) study and the Mayo Clinic Study on Aging have found no link between hypertension and brain amyloidosis. “I am glad that the UCL group came to the same conclusion,” Knopman said. In ARIC and other cohorts, researchers have reported a link between arterial stiffness, often an underlying cause of hypertension, and the accumulation of Aβ in the brain (Hughes et al., 2018; Hughes et al., 2013).
That is not to say high blood pressure poses no risk for Alzheimer’s disease. “That high blood pressure does not influence accumulation of Aβ does not, however, mean it does not influence AD,” stressed Schott. “It could affect other downstream pathologies associated with the disease, such as neuronal loss or inflammation.” In fact, results from the SPRINT MIND trial presented at AAIC show that for 60-year-olds with hypertension, lowering their systolic blood pressure to about 120 mmHg reduced incidence of mild cognitive impairment by 19 percent over 3.26 years (Aug 2018 conference news).
Schott noted that even a country-wide birth cohort study has its limitations. For example, Insight46 thus far has no postmortem or tau PET data, though 60 percent of the cohort have agreed to donate their brains.—Tom Fagan
References
News Citations
- Vascular Problems in 40s, 50s Beget Dementia Down the Road
- Blood Pressure Affects Dementia Risk Only in People Under 60
- Could Better Blood Pressure Management Preserve Cognition?
Paper Citations
- Swan GE, DeCarli C, Miller BL, Reed T, Wolf PA, Jack LM, Carmelli D. Association of midlife blood pressure to late-life cognitive decline and brain morphology. Neurology. 1998 Oct;51(4):986-93. PubMed.
- Power MC, Schneider AL, Wruck L, Griswold M, Coker LH, Alonso A, Jack CR Jr, Knopman D, Mosley TH, Gottesman RF. Life-course blood pressure in relation to brain volumes. Alzheimers Dement. 2016 Aug;12(8):890-9. Epub 2016 Apr 29 PubMed.
- Knopman DS, Penman AD, Catellier DJ, Coker LH, Shibata DK, Sharrett AR, Mosley TH Jr. Vascular risk factors and longitudinal changes on brain MRI: the ARIC study. Neurology. 2011 May 31;76(22):1879-85. Epub 2011 May 4 PubMed.
- Debette S, Seshadri S, Beiser A, Au R, Himali JJ, Palumbo C, Wolf PA, DeCarli C. Midlife vascular risk factor exposure accelerates structural brain aging and cognitive decline. Neurology. 2011 Aug 2;77(5):461-8. PubMed.
- Lane CA, Parker TD, Cash DM, Macpherson K, Donnachie E, Murray-Smith H, Barnes A, Barker S, Beasley DG, Bras J, Brown D, Burgos N, Byford M, Jorge Cardoso M, Carvalho A, Collins J, De Vita E, Dickson JC, Epie N, Espak M, Henley SM, Hoskote C, Hutel M, Klimova J, Malone IB, Markiewicz P, Melbourne A, Modat M, Schrag A, Shah S, Sharma N, Sudre CH, Thomas DL, Wong A, Zhang H, Hardy J, Zetterberg H, Ourselin S, Crutch SJ, Kuh D, Richards M, Fox NC, Schott JM. Study protocol: Insight 46 - a neuroscience sub-study of the MRC National Survey of Health and Development. BMC Neurol. 2017 Apr 18;17(1):75. PubMed.
- Petrovitch H, White LR, Izmirilian G, Ross GW, Havlik RJ, Markesbery W, Nelson J, Davis DG, Hardman J, Foley DJ, Launer LJ. Midlife blood pressure and neuritic plaques, neurofibrillary tangles, and brain weight at death: the HAAS. Honolulu-Asia aging Study. Neurobiol Aging. 2000 Jan-Feb;21(1):57-62. PubMed.
- Langbaum JB, Chen K, Launer LJ, Fleisher AS, Lee W, Liu X, Protas HD, Reeder SA, Bandy D, Yu M, Caselli RJ, Reiman EM. Blood pressure is associated with higher brain amyloid burden and lower glucose metabolism in healthy late middle-age persons. Neurobiol Aging. 2012 Apr;33(4):827.e11-9. PubMed.
- Hughes TM, Wagenknecht LE, Craft S, Mintz A, Heiss G, Palta P, Wong D, Zhou Y, Knopman D, Mosley TH, Gottesman RF. Arterial stiffness and dementia pathology: Atherosclerosis Risk in Communities (ARIC)-PET Study. Neurology. 2018 Apr 3;90(14):e1248-e1256. Epub 2018 Mar 16 PubMed.
- Hughes TM, Kuller LH, Barinas-Mitchell EJ, Mackey RH, McDade EM, Klunk WE, Aizenstein HJ, Cohen AD, Snitz BE, Mathis CA, Dekosky ST, Lopez OL. Pulse wave velocity is associated with β-amyloid deposition in the brains of very elderly adults. Neurology. 2013 Nov 5;81(19):1711-8. Epub 2013 Oct 16 PubMed.
External Citations
Further Reading
No Available Further Reading
Annotate
To make an annotation you must Login or Register.

Comments
No Available Comments
Make a Comment
To make a comment you must login or register.