Homing in on Early Alzheimer’s Biomarkers: Does Connectivity Hold the Key?
Quick Links
In the quest to find biomarkers that detect presymptomatic Alzheimer’s disease, some researchers are turning to measures of brain connectivity. Many studies have reported that functional circuits become disorganized early in the disease process, sparking interest in their potential as preclinical biomarkers. At the Alzheimer’s Association International Conference 2016, held July 22-28 in Toronto, several speakers discussed specific imaging measures that appear to flag people at the highest risk for progressing to AD. They include a gray-matter measure of connectivity, deficits in the visual network, and imaging correlates of anosognosia, which is the lack of awareness of one’s own memory problems. In a well-received talk, David Jones of the Mayo Clinic in Rochester, Minnesota, argued that network disruptions may precede and trigger amyloid and tau pathology, although the mechanism remains unknown. He put forward a method for calculating the communication breakdown based on changes in connectivity within and between subsystems of the default mode network.
Overall, researchers expressed excitement about the potential of these measures. “By describing the brain as a network, regardless of the imaging modality used, we get a more comprehensive description of brain functioning than by looking at brain areas in isolation,” Betty Tijms of VU University Medical Center, Amsterdam, wrote to Alzforum. Connectivity changes often explain cognitive problems better than do simpler measures like atrophy or hypometabolism, researchers agreed. “Network measures are really promising. I think they’ll provide us with important mechanistic interpretations of how AD progresses,” said Prashanthi Vemuri, also of the Mayo Clinic in Rochester.

Patterns of Tau Pathology.
Tangles appeared in the working memory network (left) mostly when AD struck early in life, but lit up DMN regions (right) no matter when AD developed. [Courtesy of David Jones.]
Researchers cautioned that the study of connectivity is in its infancy. It remains unclear how best to evaluate brain circuitry. Studies are exploring different types of imaging and new ways to define brain organization, and more work is needed to discover which of these are most robust. “We have to be careful to acknowledge that these measures are probably not interchangeable. ‘Connectivity’ has become an umbrella term,” Renaud La Joie of the University of California, San Francisco, wrote to Alzforum.
Currently, researchers typically measure connectivity using resting-state functional MRI. This technology maps the regions of the brain where blood flow waxes and wanes in tandem, suggesting the areas form a functional network. During the preclinical stages of AD, fMRI connectivity falters in numerous brain networks (see Jul 2012 news; Aug 2013 news; Aug 2014 news). In particular, researchers have focused on disruption of the default mode network (DMN), which is active when a person is not focused on a mental task. The DMN is one of the first networks to accumulate Aβ deposits (see Mar 2004 news; Nov 2007 news; Feb 2009 news). However, studies have not yet sorted out how network disconnection relates to pathology, and which comes first.
Could Network Failure Trigger Protein Accumulation?
Jones believes that Alzheimer’s may start with network disruptions. He previously reported cross-sectional data from a cohort of 128 ADNI participants who ranged from cognitively normal to AD dementia. Everyone in the impaired groups had amyloid accumulation, indicating they were on the path to AD. By correlating connectivity with ADAS-cog scores, which rise as people become more impaired, Jones was able to infer how brain connections changed over the course of the disease. In cognitively normal ApoE4 carriers, connectivity within the posterior DMN subsystem sputtered in the absence of any detectable amyloid plaques or brain atrophy. This network disruption appeared to trigger enhanced connectivity between other DMN subsystems, perhaps as a compensatory response. Connections between subsystems were stronger in those with worse ADAS-Cog scores. The heightened connectivity between subsystems was associated with the presence of amyloid plaques throughout the affected networks. Jones hypothesized a cascading network failure model of AD, in which synaptic disruptions themselves kindle amyloid pathology, which may then accelerate tau tangles (see Jones et al., 2016).
At AAIC, Jones proposed using this network failure pattern as a biomarker of disease. He calculated a network failure quotient (NFQ), in which the numerator represents connectivity between DMN subsystems, and the denominator, connectivity within subsystems. Because the numerator increases and the denominator drops as AD advances, their ratio rises. NFQ goes up at the preclinical stage, and correlates with changes in numerous other biomarkers, including FDG PET, amyloid and tau PET, cortical thickness, and word-list learning, Jones said.
To see if there was a relationship between network failure and molecular pathology, Jones and colleagues compared NFQ scores to amyloid PiB PET scans and AV1451 tau scans in a cohort consisting of 177 cognitively normal participants, 12 people with mild cognitive impairment, and 29 with dementia. Participants were drawn from the Mayo Clinic Study of Aging and the Mayo Clinic Alzheimer’s Disease Research Center; all of those with cognitive impairment had positive PiB scans, hence would be called amnestic MCI.
The researchers used regression analysis to determine how much of the tau pathology in their cohort could be explained by network failure, and whether tangle accumulation was mediated by amyloid. They found that two-thirds of the tau signal could be explained by the presence of amyloid. This left one-third of tau signal that associated with NFQ scores independent of amyloid. The findings support the idea that network disruptions may somehow trigger both amyloid and tau pathology, although the mechanism is unknown, Jones said. “Global network failure may lead to amyloidosis, and after saturation of amyloidosis, that network failure may then accelerate pre-existing tauopathy,” he speculated to Alzforum.
Neurofibrillary tangle deposition in this cohort occurred in specific patterns that matched three functional brain networks: the visual network, the left executive-control network, and a memory network. The first two of these accumulated tangles mostly in people with young-onset dementia. Tangles in the memory network, on the other hand, cropped up no matter when disease started, and matched the typical tau deposition patterns seen in Braak staging. This memory network overlaps with the ventral DMN, involving regions such as the medial and inferior temporal lobes and the posterior cingulate (see image above).
In each of the three networks the researchers saw a low level of tau signal even in people without biomarkers of AD, in line with neuropathological findings from older adults. Once amyloid appeared, however, the tau signal jumped throughout the entire network, with no signs of an incremental advance. On the face of it, this seems to belie theories about the gradual spread of misfolded tau along network connections. “Amyloidosis seems to accelerate an existing network-related tau abnormality,” Jones concluded. Recent tau imaging studies report that amyloid frees age-related tau pathology in the medial temporal lobe to explode throughout the cortex (see Jul 2016 news; Aug 2016 news).
An enthusiastic AAIC audience peppered Jones with questions. “The concept of tau deposition happening throughout a network is really new. We’re very excited about it,” said Vemuri, who collaborates on the research. Others were intrigued by the potential of NFQ as a biomarker. “It will be interesting to study the robustness of this measure, and how it changes over time,” Tijms said.
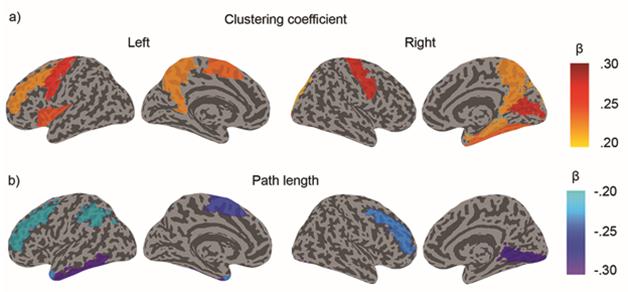
Gray Matter Connectivity Predicts AD. Disorganized gray matter (colored regions) in people with low CSF Aβ42 indicative of preclinical AD. [Courtesy of Betty Tijms.]
Faltering Connectivity Highlights Early Disease
Other talks highlighted how specific measurements of disrupted connectivity might serve as biomarkers. Tijms described a unique way to measure functional brain networks. She evaluates three-dimensional spatial relationships between neighboring voxels in a structural MRI scan. These relationships capture brain characteristics such as cortical thickness, folding, and volume, she noted. She then applies mathematical theory to calculate brain connectivity from these data (see Tijms et al., 2012). “This is based on the idea that when brain areas are involved in similar cognitive functions, they may develop in a coordinated way,” she told Alzforum. Because this method determines connectivity based on a single MRI scan instead of a lengthy resting-state fMRI session, the data are quicker and easier to obtain and suffer less from movement artifacts, Tijms said. These connectivity patterns are less pronounced in AD brains, she noted. She previously reported a correlation between disrupted gray matter connectivity and low CSF Aβ42 in cognitively healthy older adults (see Tijms et al., 2016, and image above).
Tijms wondered if the measure could single out people most at risk of progressing to AD. She analyzed data from the Connectivity in Dementia (CODA) study. This subset of the Amsterdam Dementia Cohort comprises 62 participants with subjective cognitive complaints and 160 with mild cognitive impairment, with an average age of 68. All had abnormal baseline CSF Aβ42 indicative of plaque accumulation.
Over two years, 23 of the participants with subjective complaints and 99 of those with MCI became more impaired, as measured by CDR scores. Those who progressed had weaker gray-matter connectivity at baseline than those who stayed stable, particularly between the medial temporal lobe, precuneus, posterior cortex, and inferior frontal gyrus, Tijms said. Low connectivity values throughout the brain heightened the risk of progression threefold, while deficits in those particular regions accounted for a 2.5-fold increase. “Gray-matter connectivity might be useful to predict time to AD onset,” Tijms concluded.
Other researchers made the case that specific functional brain networks may have prognostic value. Joey Annette Contreras of Indiana University, Indianapolis, correlated functional connectivity changes, as seen with resting-state fMRI, with subjective cognitive complaints in a sample from the Indiana Memory and Aging Study. Participants included 13 cognitively normal people, 16 with subjective complaints, 22 with mild cognitive impairment, and eight with Alzheimer’s disease. The more self-complaints a person reported, as measured by the Cognitive Complaint Index, the lower their connectivity in several resting-state networks, including the DMN, visual, limbic, and frontoparietal networks (see Yeo et al., 2011). In addition, the more subjective complaints a person made, this time as described by either a trusted informant or themselves, the lower the connectivity in their visual network, Contreras reported. Impaired visual memory could indicate preclinical AD, she suggested. Visual memory deficits associate with hippocampal defects and have been used to detect decline in familial AD cases (see Mar 2011 news).
Other characteristics of AD patients may point to affected networks, as well. About 80 percent of people with Alzheimer’s are unaware of their memory problems (see Lindau and Bjork, 2015). Anosognosia can also occur at the MCI stage, although data are mixed on its prevalence there (see Kalbe et al., 2005; Wilson et al., 2015).
Anosognosia at prodromal stages predicts progression to AD, Catherine Munro of Massachusetts General Hospital, Charlestown, asserted at AAIC. Among 25 people with amnestic MCI who remained stable over two years, those who performed more poorly on cognitive tests at baseline were aware of that. However, in 11 people with aMCI who progressed to AD, worse memory performance at baseline was associated with fewer memory complaints—an indication of anosognosia. Moreover, their awareness of their memory problems faded over the course of the study. In this small sample, having anosognosia ballooned the risk of progression fivefold, Munro reported.
Patrizia Vannini, also of Mass. General, investigated the brain networks underlying this phenomenon in 31 people with amnestic MCI and 31 matched controls. Anosognosia correlated with weak connectivity in parts of the DMN, particularly between the precuneus and orbitofrontal cortex, as well as the inferior parietal lobes, she reported. Weak connectivity between the precuneus and orbitofrontal cortex was particularly evident in people who progressed to AD at follow-up. Anosognosia reflects a disconnection of functional networks, Vannini concluded. In addition, people with anosognosia had hypometabolism in the posterior cingulate and right hippocampus, as Munro found, as well.
Eric Salmon of the University of Liège, Belgium, presented similar results. He correlated anosognosia in 31 AD patients with low connectivity in the memory subnetwork of the DMN. This involved the medial temporal lobe, ventral posterior cingulate cortex, posterior inferior parietal lobes, and the lateral temporal cortex. Anosognosia also went along with hypometabolism in the ventral posterior cingulate, in agreement with the Mass. General study, as well as with prior work (see Perrotin et al., 2015). This pattern makes sense, Salmon said, because portions of this memory subnetwork are responsible for a person’s ability to ponder his or her own mental state and recall past experiences (see Summerfield et al., 2009).
While various proposed connectivity measures may hold promise, validation in larger cohorts is needed to pick out good biomarkers, Vemuri noted, and Tijms agreed. “We need to identify the most robust approach to describe brain connectivity that can detect reliable differences between patients and controls across different studies and imaging modalities,” she wrote to Alzforum.—Madolyn Bowman Rogers
References
News Citations
- Communication Breakdown: Multiple Networks Decline in AD Brains
- Brain Connectivity Reveals Preclinical Alzheimer’s Disease
- Neural Circuitry Goes Haywire in Both Sporadic and Familial AD
- Network Diagnostics: "Default-Mode" Brain Areas Identify Early AD
- Functional Imaging Gives Early Glimpse of AD
- Cortical Hubs Found Capped With Amyloid
- Do Temporal Lobe Tangles and Cortical Plaques Together Bring on Alzheimer’s?
- Brain Imaging Suggests Aβ Unleashes the Deadly Side of Tau
- Detecting Familial AD Ever Earlier: Subtle Memory Signs 15 Years Before
Paper Citations
- Jones DT, Knopman DS, Gunter JL, Graff-Radford J, Vemuri P, Boeve BF, Petersen RC, Weiner MW, Jack CR Jr, Alzheimer’s Disease Neuroimaging Initiative. Cascading network failure across the Alzheimer's disease spectrum. Brain. 2016 Feb;139(Pt 2):547-62. Epub 2015 Nov 19 PubMed.
- Tijms BM, Seriès P, Willshaw DJ, Lawrie SM. Similarity-based extraction of individual networks from gray matter MRI scans. Cereb Cortex. 2012 Jul;22(7):1530-41. Epub 2011 Aug 30 PubMed.
- Tijms BM, ten Kate M, Wink AM, Visser PJ, Ecay M, Clerigue M, Estanga A, Garcia Sebastian M, Izagirre A, Villanua J, Martinez Lage P, van der Flier WM, Scheltens P, Sanz Arigita E, Barkhof F. Gray matter network disruptions and amyloid beta in cognitively normal adults. Neurobiol Aging. 2016 Jan;37:154-60. Epub 2015 Oct 22 PubMed.
- Yeo BT, Krienen FM, Sepulcre J, Sabuncu MR, Lashkari D, Hollinshead M, Roffman JL, Smoller JW, Zöllei L, Polimeni JR, Fischl B, Liu H, Buckner RL. The organization of the human cerebral cortex estimated by intrinsic functional connectivity. J Neurophysiol. 2011 Sep;106(3):1125-65. Epub 2011 Jun 8 PubMed.
- Lindau M, Bjork R. Anosognosia and anosodiaphoria in mild cognitive impairment and Alzheimer's disease. Dement Geriatr Cogn Dis Extra. 2014 Sep-Dec;4(3):465-80. Epub 2014 Dec 3 PubMed.
- Kalbe E, Salmon E, Perani D, Holthoff V, Sorbi S, Elsner A, Weisenbach S, Brand M, Lenz O, Kessler J, Luedecke S, Ortelli P, Herholz K. Anosognosia in very mild Alzheimer's disease but not in mild cognitive impairment. Dement Geriatr Cogn Disord. 2005;19(5-6):349-56. PubMed.
- Wilson RS, Boyle PA, Yu L, Barnes LL, Sytsma J, Buchman AS, Bennett DA, Schneider JA. Temporal course and pathologic basis of unawareness of memory loss in dementia. Neurology. 2015 Sep 15;85(11):984-91. Epub 2015 Aug 26 PubMed.
- Perrotin A, Desgranges B, Landeau B, Mézenge F, La Joie R, Egret S, Pélerin A, de la Sayette V, Eustache F, Chételat G. Anosognosia in Alzheimer disease: Disconnection between memory and self-related brain networks. Ann Neurol. 2015 Sep;78(3):477-86. Epub 2015 Jul 21 PubMed.
- Summerfield JJ, Hassabis D, Maguire EA. Cortical midline involvement in autobiographical memory. Neuroimage. 2009 Feb 1;44(3):1188-200. Epub 2008 Oct 10 PubMed.
Further Reading
No Available Further Reading
Annotate
To make an annotation you must Login or Register.

Comments
No Available Comments
Make a Comment
To make a comment you must login or register.