TREM2 Tidbits at AAIC: Genetics, Clinical Data
Quick Links
TREM2 mutations raise one’s risk for Alzheimer’s disease—but which variants cause problems, and how? Researchers wrestling with these questions presented their latest results at the Alzheimer’s Association International Conference 2015, held July 18-23 in Washington, D.C. Many have been hampered by the extreme rarity of TREM2 variants, which meant they could only collect a handful of subjects for their work. Scientists have yet to come to agreement on whether TREM2 mutations can cause neurodegenerative conditions beyond Alzheimer’s, and how the gene contributes to neuropathology.
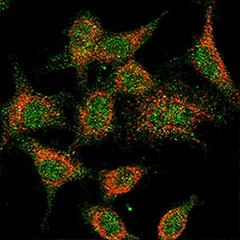
Microglia make TREM2 (red), which can be detected on the cell surface (green). [Courtesy of Konstantin Glebov and Patrick Wunderlich, University of Bonn.]
Mutations in TREM2 were discovered in people with frontotemporal lobar degeneration or Alzheimer’s disease in 2012 (see Oct 2012 news; Nov 2012 news). The gene has also been linked to ALS, leading scientists to wonder if it might be a general neurodegeneration risk factor (Feb 2014 news). However, the full picture of TREM2 and disease risk remains uncertain, in part due to small studies with conflicting results. According to a recent meta-analysis by Lars Bertram and Christina Lill of the University of Lübeck in Germany, published online April 30 in Alzheimer’s & Dementia, an arginine-47-histidine (R47H) substitution in the gene enlarges a person’s risk of Alzheimer’s by a factor of 2.71. The authors’ dataset included 24,086 AD cases, plus 2,673 people with FTLD, 8,311 with Parkinson’s, and 5,544 with ALS. They were unable to confirm a significant link between the R47H variant and FTD, ALS, or PD, though it remains possible that other TREM2 mutations contribute to those diseases.
Indeed, researchers have not completely catalogued the variety possible in TREM2 sequences, nor which variants are pathogenic. At AAIC, Alfredo Ramirez of the University of Bonn, Germany, reported preliminary data on a new variant likely involved in Alzheimer’s. Though he would not reveal the specific mutation, he told Alzforum it occurred in the extracellular portion of the protein. Ramirez and colleagues discovered the variant in two members of a Portuguese family diagnosed with an inherited form of AD, who had no APP or PS mutations and were ApoE4-negative. They could not detect the TREM2 variant in an unaffected relative or in 1,400 people with sporadic AD. Two other family members share the variant. One, who is 61, shows no signs of dementia, while the other, who is 50 years old, has had mild cognitive problems for 10 years.
Jochen Walter, also at the University of Bonn, investigated the function of the new variant. It ran faster on polyacrylamide gels, suggesting it was structurally different from the wild-type protein, but Ramirez said he detected no post-translational modification and he suspects the protein folds differently. They also examined shedding of the extracellular portion of TREM2, which occurs when microglia are active. When they expressed TREM2 constructs in HEK293 cells, the variant shed twice as much extracellular domain into the culture medium as did wild-type TREM2. In support of this, the researchers detected less of the variant on the cell surface.
TREM2 activation leads to internal cellular signaling that remodels the actin cytoskeleton and causes cells to round up, reducing their surface area. Since scientists have yet to find a ligand for TREM2, Konstantin Glebov and Patrick Wunderlich in Walter’s lab mimicked one by adding an anti-Myc antibody to COS cells expressing TREM2 with an N-terminal Myc tag. Surface area of cells expressing normal TREM2 modified in this way shrank on addition of the antibody, while it had no effect on cells producing the variant TREM2 with the N-terminal Myc tag. This ties in with heightened shedding of the variant, said Ramirez.
Amanda Heslegrave of University College London reported on TREM2 in the CSF. The receptor’s extracellular domain, shed from the microglia membrane after cleavage by γ-secretase, winds up in the spinal fluid. Scientists do not fully understand why TREM2 shedding occurs, said study co-author Henrik Zetterberg of the University of Gothenburg in Sweden. Might TREM2 in the CSF indicate something about the disease processes, or even serve as a biomarker?
Heslegrave and colleagues analyzed TREM2, Aβ, and tau in CSF from 34 people with AD who had a normal TREM2 genotype, and 20 cognitively normal controls. They struggled to obtain reproducible results from antibody-based assays for TREM2, so they switched to a mass-spectrometry method, quantifying a peptide unique to the TREM2 extracellular domain. They found the concentration of this peptide, VLVEVLADPLDHR, was higher in people with AD, and correlated with that of tau but not Aβ. Since CSF tau reflects injured neurons, the authors speculate that increased TREM2 shedding indicates that microglia are activated, yet ineffective at protecting the brain.
Zetterberg told Alzforum that TREM2 could be a potential biomarker for microglial activation, but probably would not be specific for AD. The researchers plan to examine TREM2 in longitudinal CSF samples to better understand how it changes with disease course, he said.
A separate study run by Christian Haass at Ludwig-Maximilians University in Munich used a TREM2 ELISA assay in more than 800 CSF samples from people who are cognitively normal, preclinical, prodromal or AD patients. This ongoing study also finds soluble TREM2 in CSF to be increased, particularly at the prodromal stage. The TREM2 elevation correlates with elevated CSF tau, indicating TREM2 could become a biomarker for an early inflammatory stage in AD pathogenesis.
In their paper, Lill and Bertram reported that TREM2 R47H carriers exhibited elevated CSF tau, corroborating the link between the two molecules.
Other researchers at the meeting investigated how known TREM2 variants affected Alzheimer’s onset and cognitive symptoms. Corinne Engelman of the University of Wisconsin School of Medicine and Public Health in Madison focused on R47H carriers. Engelman works with the longitudinal Wisconsin Registry for Alzheimer’s Prevention (WRAP) cohort. Most WRAP participants are too young to have developed dementia, but about two-thirds had a parent with the disease, and the data set includes clinical information from those participants. Among 1,200 of the cohort, Engelman discovered 10 carriers of R47H TREM2. Each had a family history of AD, though she has not checked yet to see if they themselves exhibited dementia symptoms. Their mothers' ages at disease onset averaged 66 years old—eight years younger than for affected mothers of non-carriers in this cohort. Without genetic data from the carriers’ parents, Engelman cannot be sure if any were also R47H carriers. Even so, her results are consistent with other work suggesting that TREM2 variants can speed up and worsen disease, Engelman said.
For fathers, however, onset occurred about six months earlier, which was not statistically significant. Engelman speculated that TREM2 variants may have a stronger effect in women, but she cautioned that her sample contained only four fathers, but seven mothers, meaning the difference may be due to chance. In six different tests of cognitive function, the 10 R47H carriers tended to perform slightly worse than non-carriers, but this difference was not statistically significant either.
Alexander Koppara, also at the University of Bonn, and Ramirez investigated the role of R47H and six other TREM2 variants in late-onset AD in the prospective AgeCoDe study (Luck et al., 2007). A 2014 paper had reported that in cases of early onset AD, R47H hastened the first symptoms by six years (Slattery et al., 2014), and one of the first studies to link TREM2 and AD indicated that R47H carriers fared worse, cognitively, than non-carriers in a cross-sectional cohort (Jonsson et al., 2013). Koppara found that among 10 carriers with dementia (eight female) and 270 matched non-carriers in AgeCoDe, TREM2 genotype made no difference to age of onset. They also examined Mini Mental State Examination (MMSE) scores and found that TREM2 mutation status did not affect the rate of decline.
In another poster, Klaus Fliessbach, also of the University of Bonn, reported a case study of a person with a threonine-96-lysine substitution in TREM2, which researchers suspected to be pathogenic. This person had cerebrospinal fluid (CSF) and PiB-PET imaging, and symptoms of the logopenic variant of primary progressive aphasia (lvPPA), which is characterized by difficultly retrieving words. Usually, people with lvPPA progress quickly, but this disease advanced slowly. Five years after the first symptoms, the patient was still able to live independently and scored 28 out of 30 on the MMSE. “The case is an example of an extremely benign clinical course in lvPPA,” the authors concluded. “We suggest that the investigation of genetics and other disease-modifying variables underlying the clinical variability in lvPPA progression is an important target for future research.”
The overall picture of TREM2 and AD remains murky for the time being, researchers told Alzforum. “The genetic findings are still too recent for us to have a firm and established idea of what TREM2 is doing,” Bertram said. “Clearly the immune system is involved, but it is not clear how.”—Amber Dance
References
News Citations
- Mutations in TREM2 Cause Frontotemporal Dementia
- Enter the New Alzheimer’s Gene: TREM2 Variant Triples Risk
- TREM2 Variant Doubles the Risk of ALS
Paper Citations
- Luck T, Riedel-Heller SG, Kaduszkiewicz H, Bickel H, Jessen F, Pentzek M, Wiese B, Koelsch H, van den Bussche H, Abholz HH, Moesch E, Gorfer S, Angermeyer MC, Maier W, Weyerer S, AgeCoDe group. Mild cognitive impairment in general practice: age-specific prevalence and correlate results from the German study on ageing, cognition and dementia in primary care patients (AgeCoDe). Dement Geriatr Cogn Disord. 2007;24(4):307-16. Epub 2007 Sep 11 PubMed.
- Slattery CF, Beck JA, Harper L, Adamson G, Abdi Z, Uphill J, Campbell T, Druyeh R, Mahoney CJ, Rohrer JD, Kenny J, Lowe J, Leung KK, Barnes J, Clegg SL, Blair M, Nicholas JM, Guerreiro RJ, Rowe JB, Ponto C, Zerr I, Kretzschmar H, Gambetti P, Crutch SJ, Warren JD, Rossor MN, Fox NC, Collinge J, Schott JM, Mead S. R47H TREM2 variant increases risk of typical early-onset Alzheimer's disease but not of prion or frontotemporal dementia. Alzheimers Dement. 2014 Nov;10(6):602-608.e4. Epub 2014 Aug 23 PubMed.
- Jonsson T, Stefansson H, Steinberg S, Jonsdottir I, Jonsson PV, Snaedal J, Bjornsson S, Huttenlocher J, Levey AI, Lah JJ, Rujescu D, Hampel H, Giegling I, Andreassen OA, Engedal K, Ulstein I, Djurovic S, Ibrahim-Verbaas C, Hofman A, Ikram MA, van Duijn CM, Thorsteinsdottir U, Kong A, Stefansson K. Variant of TREM2 associated with the risk of Alzheimer's disease. N Engl J Med. 2013 Jan 10;368(2):107-16. Epub 2012 Nov 14 PubMed.
External Citations
Further Reading
Papers
- Tanzi RE. TREM2 and Risk of Alzheimer's Disease--Friend or Foe?. N Engl J Med. 2015 Jun 25;372(26):2564-5. PubMed.
- Jin SC, Benitez BA, Karch CM, Cooper B, Skorupa T, Carrell D, Norton JB, Hsu S, Harari O, Cai Y, Bertelsen S, Goate AM, Cruchaga C. Coding variants in TREM2 increase risk for Alzheimer's disease. Hum Mol Genet. 2014 Nov 1;23(21):5838-46. Epub 2014 Jun 4 PubMed.
- Engelman CD, Koscik RL, Jonaitis EM, Hermann BP, La Rue A, Sager MA. Investigation of triggering receptor expressed on myeloid cells 2 variant in the Wisconsin Registry for Alzheimer's Prevention. Neurobiol Aging. 2014 Jun;35(6):1252-4. Epub 2013 Nov 20 PubMed.
Primary Papers
- Lill CM, Rengmark A, Pihlstrøm L, Fogh I, Shatunov A, Sleiman PM, Wang LS, Liu T, Lassen CF, Meissner E, Alexopoulos P, Calvo A, Chio A, Dizdar N, Faltraco F, Forsgren L, Kirchheiner J, Kurz A, Larsen JP, Liebsch M, Linder J, Morrison KE, Nissbrandt H, Otto M, Pahnke J, Partch A, Restagno G, Rujescu D, Schnack C, Shaw CE, Shaw PJ, Tumani H, Tysnes OB, Valladares O, Silani V, van den Berg LH, van Rheenen W, Veldink JH, Lindenberger U, Steinhagen-Thiessen E, SLAGEN Consortium, Teipel S, Perneczky R, Hakonarson H, Hampel H, von Arnim CA, Olsen JH, Van Deerlin VM, Al-Chalabi A, Toft M, Ritz B, Bertram L. The role of TREM2 R47H as a risk factor for Alzheimer's disease, frontotemporal lobar degeneration, amyotrophic lateral sclerosis, and Parkinson's disease. Alzheimers Dement. 2015 Dec;11(12):1407-1416. Epub 2015 Apr 30 PubMed.
Annotate
To make an annotation you must Login or Register.

Comments
No Available Comments
Make a Comment
To make a comment you must login or register.