Popcorn Plaque? Alzheimer Disease Is Slow, Yet Plaque Growth Is Fast
Quick Links
Thanks to a new imaging technology that enables an investigator to peer again and again into the same brain area of a live mouse without disturbing it, researchers discovered that amyloid plaques, one pathologic hallmark of Alzheimer disease, can literally show up overnight and grow to their full size in just a few days. The study addresses long-standing questions about the sequence of pathogenic changes in the brain, and it affords scientists a more immediate look at those changes than was possible before. In the February 7 Nature, Melanie Meyer-Luehmann, Tara Spires-Jones, and others in Brad Hyman’s group at Massachusetts General Hospital in Charlestown collaborated with David Holtzman’s group at Washington University, St. Louis, Missouri, to generate vivid three-color images of new plaques popping up between daily imaging sessions. Soon after a plaque precipitated, the scientists saw microglia moving in and kinks appearing in nearby neurites.
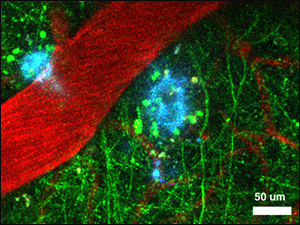
Two amyloid-β plaques (blue), neurites expressing yellow fluorescent protein (green), and blood vessels (red), taken in B6C3 mouse. Image credit: Melanie Meyer-Luehmann.
The speed at which plaques arise surprised the scientists, because the established knowledge that Alzheimer disease pathology takes years to accumulate in a person’s brain had led to a general assumption that individual plaques grow slowly. In contrast, the new work shows that once the predominant constituent of a plaque, Aβ protein, has accumulated to sufficient amounts, the deposition of a plaque happens quickly. By implication, the overall growth of the brain’s plaque load would be a long process made up of many local cycles of rapid deposition of a new plaque followed by rapid change in the microenvironment around the new plaque. The present study does not address the role of oligomeric Aβ species, as those cannot yet be imaged in live brain. Neither did it probe whether the newly appearing plaques affect neural activity.
The study directly addresses the question of how plaques form and whether certain other changes in the vicinity of plaques occur before or after a plaque has formed. In this sense, the study aims to test the amyloid hypothesis in its classic form, which claims that amyloid deposition precedes and causes neuronal abnormalities that then lead to dementia.
The Hyman lab has been at the forefront of developing in-vivo multiphoton microscopy techniques for the study of AD. Here the scientist permanently places a glass cover over a small hole in a mouse’s skull, and through this window images the same area of cortex repeatedly over the course of weeks. In this study, Meyer-Luehmann and colleagues used three different mouse models of AD amyloidosis to watch plaques grow. They used APP-transgenic mouse strains that also express YFP in neurons to visualize neurites, dendrites, and axons in the neuropil, injected the amyloid dye methoxy-XO4 to render fibrillar plaques blue, and the dye Texas red dextran to label blood vessels. Existing plaques and blood vessels served as guideposts to orient the scientists, and helped them re-image the same area they had seen the day or week before. Overall, the scientists found existing plaques to be stable over the 1,285 imaging sessions they conducted on 238 brain sites in 14 mice. On 26 occasions, however, they captured the growth of a new plaque in those repeat sessions. Some imaging series were weekly, others daily; the latter revealed five new plaques, each appearing in a 24-hour time span, the researchers report.
New plaques grew little after their “birthday.” They were similar in size to plaques measured in postmortem tissue, most of them being between 5 and 20 micrometers wide. The scientists also looked at where new plaques cropped up in relation to blood vessels. They report that the 26 new plaques tended to form near but not directly on or around blood vessels. In prior studies of older APP- or presenilin-transgenic mice, blood vessels have been seen to be tightly associated with plaques or course right through them, raising the possibility that the brain’s microvasculature has a direct role in plaque formation (Kumar-Singh et al., 2005; ARF related news story; see also Kumar-Singh comment below).
Next, the scientists analyzed the new plaques with regard to two parameters in their local environment, namely microglia and neurites. Within a day of a plaque’s appearance, the scientists noted that microglia moved in next to it, suggesting that perhaps some factors released from the plaque had recruited these cells. However, Meyer-Luehmann et al. never observed neighboring microglia nibble into an adjacent plaque. The role of microglia in AD pathogenesis is uncertain, and phagocytosis of plaques is one of the roles that prior research has proposed. The present data imply that microglia may need to be activated further, such as by an immunotherapy, to actually ingest and remove amyloid plaques (Bacskai et al., 2001). The level of microglial activation seen in the current study might explain why the plaques barely grow after their initial appearance, the scientists speculate. Other studies have suggested that activated microglia limit plaque growth (Simard et al., 2006).
Like microglia, neurites in the neighborhood of a newly formed plaque also responded within the same time frame of between a day and a week after a plaque had appeared. Where these neurites were previously straight or bending smoothly, they became more curved and twisted. Recent work from Larry Goldstein’s group at the University of California, San Diego, had suggested that defects in axonal transport—recognizable morphologically as misshapen, or dystrophic neurites—precede amyloid pathology and can accelerate the formation of plaques (Stokin et al., 2005). The present study was unable to see plaques forming in areas that had prominent neuritic dystrophy; instead, it suggests that neurites become distorted after a plaque has formed. However, the authors do not rule out the importance of axonal transport changes in AD pathogenesis (see also Goldstein comment below).
Overall, the study provides a glimpse into the dynamic changes in the brain of AD mouse models. The technique allows scientists to watch from deposition onward what happens near a plaque. Meyer-Luehmann and colleagues see plaques as the source of soluble Aβ and possibly other bioactive molecules—indeed, many AD scientists talk about plaques as “leaching toxic waste dumps.” The important question of whether a newly formed plaque changes neural activity in its immediate environment remains to be tackled.
In AD mouse models, numerous studies have documented learning and memory deficits prior to plaque formation, whereas in humans, amyloid imaging suggests that pathology appears to be nearly complete before people are diagnosed with AD. This discrepancy leaves still unsolved the larger “chicken-and-egg” dilemma about the sequence of events around Aβ accumulation and dementia, even as it establishes that plaque formation precedes microglial activation and derangement of neurites in these models. New live imaging tools (see Bar Harbor report) are needed to assess the role of amyloid on function and to probe what role Aβ oligomers, and other factors, may play prior to plaque deposition.—Gabrielle Strobel
Q&A with Brad Hyman. Questions by Gabrielle Strobel.
Q: My jaw fairly dropped at how quickly the plaques appear. You report it in three different mouse models. Still, can you be sure that it is not an artifact of some experimental manipulation?
A: While we cannot be certain, the three models we used have greatly differing tempos (onset varying from 6 months to 14 months), so we think that the rapid plaque formation occurs independently of the tempo of the model.
Q: Some readers may interpret your findings as, "So it's the plaques, after all." Does your new finding promote a hypothesis of plaque toxicity at the expense of oligomer toxicity?
A: The "halo" effect suggests that there is a bioactive, diffusible substance that is high near plaques. While we have not identified this species with certainty, oligomeric Aβ is a great candidate. We think this is more an issue of "both" rather than "either."
Q: Most scientists at this point agree that both plaques and oligomers/protofibrils are bad. Is the relationship between toxicity attributable to specific aggregation forms of Aβ still an important question?
A: Of course!
Q: Do you intend to address it in this system?
A: We are testing reagents that might give a handle on oligomeric forms, but do not have data yet.
Q: Are there any tools on the horizon to image oligomers in vivo?
A: (Maybe!)
Q: You propose that plaques are a source of toxic oligomers, which might damage neurites. But presumably, oligomers were present in the brain parenchyma before the day the plaque precipitated, and present at high concentration if one assumes they accumulate to a certain point and then “crash” out of solution into a plaque. Why would oligomers not have caused the curved neurites, activated microglia, and done other bad things before the plaque showed up? Why in the 5 days after the plaque?
A: These are great questions.
Q: Trying to find out which aspects of microglial activation are detrimental and which might indeed be compensatory is a complicated issue in the field. What's the upshot of your paper on that question?
A: I think you have put your finger on one of the issues that we need to focus on—it is a complicated but fascinating set of questions.
Q: Where does evidence for axonal transport deficits still fit into your observations? Do you see it as secondary to amyloid pathology?
A: We are launching a series of experiments explicitly testing the idea that axon transport is altered near plaques.
Q: Do your findings have implications for current anti-amyloid drug development approaches?
A: Our data suggest that a viable target would be the nucleation phenomenon, and also that plaques per se are an important target.
Q: How about anti-inflammatory approaches?
A: The apparent role of microglia in stopping further growth of plaques would seem to indicate that some aspects of microglial activation might be beneficial.
Q: What's next in your line of research?
A: Understanding the functional consequences of plaque formation.
References
News Citations
Paper Citations
- Kumar-Singh S, Pirici D, McGowan E, Serneels S, Ceuterick C, Hardy J, Duff K, Dickson D, Van Broeckhoven C. Dense-core plaques in Tg2576 and PSAPP mouse models of Alzheimer's disease are centered on vessel walls. Am J Pathol. 2005 Aug;167(2):527-43. PubMed.
- Bacskai BJ, Kajdasz ST, Christie RH, Carter C, Games D, Seubert P, Schenk D, Hyman BT. Imaging of amyloid-beta deposits in brains of living mice permits direct observation of clearance of plaques with immunotherapy. Nat Med. 2001 Mar;7(3):369-72. PubMed.
- Simard AR, Soulet D, Gowing G, Julien JP, Rivest S. Bone marrow-derived microglia play a critical role in restricting senile plaque formation in Alzheimer's disease. Neuron. 2006 Feb 16;49(4):489-502. PubMed.
- Stokin GB, Lillo C, Falzone TL, Brusch RG, Rockenstein E, Mount SL, Raman R, Davies P, Masliah E, Williams DS, Goldstein LS. Axonopathy and transport deficits early in the pathogenesis of Alzheimer's disease. Science. 2005 Feb 25;307(5713):1282-8. PubMed.
Other Citations
Further Reading
Primary Papers
- Meyer-Luehmann M, Spires-Jones TL, Prada C, Garcia-Alloza M, de Calignon A, Rozkalne A, Koenigsknecht-Talboo J, Holtzman DM, Bacskai BJ, Hyman BT. Rapid appearance and local toxicity of amyloid-beta plaques in a mouse model of Alzheimer's disease. Nature. 2008 Feb 7;451(7179):720-4. PubMed.
Annotate
To make an annotation you must Login or Register.

Comments
University of Antwerp
This is another state-of-the-art paper by the group active on in vivo two-photon imaging on mouse models of amyloidogenesis, and it gives important clues for Alzheimer disease pathogenesis. The paper shows, for the first time, that dense plaques in mouse models reach their maximum size in about a day and thereafter maintain a status quo. This does not follow the simple, size-dependent law of mass action, as even small plaques do not grow any further. This is a most amazing finding and abrogates all prior preconceived notions that plaques grow slowly over life and that given time, all plaques would reach a maximum size. Importantly, the quick growth of dense plaques suggests that dense plaques grow not only with Aβ monomer addition, but perhaps also by capturing oligomeric intermediates at the fiber ends, as shown earlier for prion proteins (Serio et al., 2000; Collins et al., 2004).
Why dense plaques stop growing suddenly is just as intriguing. Quick recruitment of macrophages at sites of dense plaque formation, as shown here, could be one mechanism, but the provided images do not show a complete walling off. This suggests that other, less simple mechanisms are at play, including local Aβ production and trafficking.
A recent, interesting study in a mouse model of amyloidogenesis showed that FAD APP mutations cause axonal trafficking defects and that that, in turn, stimulates the proteolytic processing of APP and generation of Aβ (Stokin et al., 2005). This fit well with development of dystrophic neurites (DNs) in these mice, preceding plaques by more than a year (Stokin et al., 2005). Meyer-Luehmann and colleagues, studying the temporal relation between rapidly growing plaques and DNs, showed that although DNs were observed in plaque-free areas, DNs were more pronounced near plaques. Conversely, DNs in the plaque-free areas did not seem to cause dense plaques, and mice did not deposit diffuse plaques at this age. It would be worth studying this in more detail over a shorter time window, as DNs were also observed to change morphologies and even resolve, leaving open the possibility that diffuse or pre-diffuse plaques are formed but are quickly turned over. Moreover, the current resolution of this technique does not permit visualization of small, dense plaques, and at times it leaves the reader guessing whether some of the punctate blue staining might potentially be “sub-microscopic” dense plaques (for instance, boxed areas in Figure 1). Also, sometimes the capillary network is strangely absent, for instance, some panels of Figure 1 representing APPswe/PS1d9xYFP mice, where the plaque-vessel relationship has been alluded to on a small sample size.
Clearly, more work is needed before we can have all the answers. Meanwhile, despite some of its limitations, in vivo multiphoton imaging remains a valuable technique. We hope to see more results coming out from this technology, especially with higher objectives, use of confocal settings, and perhaps a shorter time lapse, even though that would make it even more labor-intensive. Parallel detailed histological analysis including ultrastructural microscopy should make it even more interesting.
References:
Collins SR, Douglass A, Vale RD, Weissman JS. Mechanism of prion propagation: amyloid growth occurs by monomer addition. PLoS Biol. 2004 Oct;2(10):e321. PubMed.
Meyer-Luehmann M, Spires-Jones TL, Prada C, Garcia-Alloza M, de Calignon A, Rozkalne A, Koenigsknecht-Talboo J, Holtzman DM, Bacskai BJ, Hyman BT. Rapid appearance and local toxicity of amyloid-beta plaques in a mouse model of Alzheimer's disease. Nature. 2008 Feb 7;451(7179):720-4. PubMed.
Serio TR, Cashikar AG, Kowal AS, Sawicki GJ, Moslehi JJ, Serpell L, Arnsdorf MF, Lindquist SL. Nucleated conformational conversion and the replication of conformational information by a prion determinant. Science. 2000 Aug 25;289(5483):1317-21. PubMed.
Spires TL, Meyer-Luehmann M, Stern EA, McLean PJ, Skoch J, Nguyen PT, Bacskai BJ, Hyman BT. Dendritic spine abnormalities in amyloid precursor protein transgenic mice demonstrated by gene transfer and intravital multiphoton microscopy. J Neurosci. 2005 Aug 3;25(31):7278-87. PubMed.
Stokin GB, Lillo C, Falzone TL, Brusch RG, Rockenstein E, Mount SL, Raman R, Davies P, Masliah E, Williams DS, Goldstein LS. Axonopathy and transport deficits early in the pathogenesis of Alzheimer's disease. Science. 2005 Feb 25;307(5713):1282-8. PubMed.
View all comments by Samir Kumar-Singh�
Meyer-Luehmann et al. provide a spectacular and informative high-tech view of the kinetics of amyloid formation and its potential consequences in a mouse model of Alzheimer disease. Although some may regard their findings as contradictory to the idea that early transport defects may play a role in neuronal dysfunction and in the enhancement of amyloid formation in Alzheimer disease, I do not see this study as being in conflict with those ideas. There are two major points:
1. In addition to the experiments we reported (Stokin et al., 2005), there are a number of previous studies (cited in Stokin et al., 2005) that find significant axonal dystrophies, which may be indicative of defects in axonal transport, prior to amyloid deposition as well as in regions of the brain that lack amyloid deposition. A related issue is that the experiments of Meyer-Luehmann et al. primarily focus on cortical regions, while many of the experiments in Stokin et al. examined basal forebrain cholinergic axons, which are long projection axons in regions distinct from the cortical regions imaged in the present paper.
2. A number of papers (Torroja et al., 1999; Gunawardena et al., 2001; Salehi et al., 2006; Pigino et al., 2003) report that APP overexpression and presenilin mutations, both of which can cause Alzheimer disease, can induce serious abnormalities in axonal transport in the absence of plaque formation or human Aβ. Again, these findings and those of Meyer-Luehmann et al. are not in conflict and may in some sense be complementary.
A possibly useful way to think about this collection of observations is by asking two questions: 1) Are amyloid plaques completely benign? 2) Are amyloid plaques or their constituents sufficient to induce all of the biochemical and cellular malfunctions associated with Alzheimer disease? The answer to the first question is almost surely no—it is hard to imagine that massive numbers of amyloid plaques in the brain would not interfere with neuronal function. Indeed, there is ample documentary evidence that amyloid constituents can be neurotoxic to varying degrees. The answer to the second question is far from clear. APP processing clearly generates fragments other than Aβ, and may influence other biological activities of APP and neurons. It may be that a productive additional approach to this question is by trying to understand the relative toxicity of Aβ to neurons compared to toxicity caused by other environmental influences, mutations, pathways, or polymorphisms that all may reduce or impair the supply of critical materials to synapses by the axonal transport machinery.
References:
Stokin GB, Lillo C, Falzone TL, Brusch RG, Rockenstein E, Mount SL, Raman R, Davies P, Masliah E, Williams DS, Goldstein LS. Axonopathy and transport deficits early in the pathogenesis of Alzheimer's disease. Science. 2005 Feb 25;307(5713):1282-8. PubMed.
Torroja L, Chu H, Kotovsky I, White K. Neuronal overexpression of APPL, the Drosophila homologue of the amyloid precursor protein (APP), disrupts axonal transport. Curr Biol. 1999 May 6;9(9):489-92. PubMed.
Gunawardena S, Goldstein LS. Disruption of axonal transport and neuronal viability by amyloid precursor protein mutations in Drosophila. Neuron. 2001 Nov 8;32(3):389-401. PubMed.
Salehi A, Delcroix JD, Belichenko PV, Zhan K, Wu C, Valletta JS, Takimoto-Kimura R, Kleschevnikov AM, Sambamurti K, Chung PP, Xia W, Villar A, Campbell WA, Kulnane LS, Nixon RA, Lamb BT, Epstein CJ, Stokin GB, Goldstein LS, Mobley WC. Increased App expression in a mouse model of Down's syndrome disrupts NGF transport and causes cholinergic neuron degeneration. Neuron. 2006 Jul 6;51(1):29-42. PubMed.
Pigino G, Morfini G, Pelsman A, Mattson MP, Brady ST, Busciglio J. Alzheimer's presenilin 1 mutations impair kinesin-based axonal transport. J Neurosci. 2003 Jun 1;23(11):4499-508. PubMed.
View all comments by Larry GoldsteinThis is a beautiful paper showing plaque growth in vivo. I cordially disagree on one point: the authors state that the speed of an individual plaque's growth is surprising because of prior in vitro studies of protein aggregation showing a slow, time-dependent course. The discussion appears to suggest that the appearance of a plaque within a day or two does not fit in with data on nucleation-dependent polymerization (Jarrett and Lansbury, 1993). In fact, the observations in this paper are reminiscent of seeded crystal growth. Live multiphoton imaging cannot yet visualize the prior accumulation of Aβ or the nucleation event, but once nucleation happens, growth should be very fast. The rate of growth measured in this study is exactly what the nucleation model would predict. It is gratifying to see in vivo.
References:
Jarrett JT, Lansbury PT. Seeding "one-dimensional crystallization" of amyloid: a pathogenic mechanism in Alzheimer's disease and scrapie?. Cell. 1993 Jun 18;73(6):1055-8. PubMed.
View all comments by Peter LansburyUniversity of California San Diego
This paper is intriguing, to say the least. The authors succeeded in monitoring in vivo the formation of dense-core plaques. Surprisingly, they observed that across different mouse models of Alzheimer disease, plaques formed quite rapidly (24 hours) but rarely. One of the most interesting observations of the paper is the temporal relation between rapid dense-core plaque appearance, microglial recruitment, and neuritic changes. Morphological changes of neurites never preceded plaque appearance and/or microglia migration towards the site of the newly formed plaque. Microglia did not seem to either facilitate or clear plaques, suggesting that they may participate in stabilizing plaque size after their initial acute growth.
If we consider that, in recent years, soluble Aβ oligomers rather than Aβ fibrils in plaques have come to be seen as the “real bad guys” (Walsh and Selkoe, 2007), these new findings raise nearly as many questions as they answer. For example, are the neuritic alterations described in this paper induced by soluble forms of amyloid-β or by plaques themselves? If the former, why would soluble Aβ oligomers be responsible for dysmorphic neurites only when released by the plaques, but not as precursors of the same plaques? And even if we assume that these newly formed plaques function just as a local source of highly concentrated soluble Aβ, then why would dystrophic neurites take several days to appear? Faster morphological, functional, and behavioral alterations induced by soluble Aβ oligomers have been described both in cultured neurons (Calabrese et al., 2007), slices (Klyubin et al., 2005; Shankar et al., 2007), and in living rats (Cleary et al., 2005).
To prove a direct role for plaques in inducing morphological changes, one would have to show that a selectively induced disassembly of the dense-core plaques would result in microglia dispersion and restoration of normal neurites. Recently, Martins et al. (2008) have shown that biologically relevant lipids, including lipid extracts from brain, can revert inert Aβ amyloid fibrils into neurotoxic protofibrils. Microglia could use a similar mechanism to control the size of amyloid-β plaques.
Finally, the biggest challenge will be to identify the predictors for such sudden and local appearance of amyloid-β plaques so that eventually their formation can be prevented.
References:
Calabrese B, Shaked GM, Tabarean IV, Braga J, Koo EH, Halpain S. Rapid, concurrent alterations in pre- and postsynaptic structure induced by naturally-secreted amyloid-beta protein. Mol Cell Neurosci. 2007 Jun;35(2):183-93. PubMed.
Cleary JP, Walsh DM, Hofmeister JJ, Shankar GM, Kuskowski MA, Selkoe DJ, Ashe KH. Natural oligomers of the amyloid-beta protein specifically disrupt cognitive function. Nat Neurosci. 2005 Jan;8(1):79-84. PubMed.
Klyubin I, Walsh DM, Lemere CA, Cullen WK, Shankar GM, Betts V, Spooner ET, Jiang L, Anwyl R, Selkoe DJ, Rowan MJ. Amyloid beta protein immunotherapy neutralizes Abeta oligomers that disrupt synaptic plasticity in vivo. Nat Med. 2005 May;11(5):556-61. PubMed.
Martins IC, Kuperstein I, Wilkinson H, Maes E, Vanbrabant M, Jonckheere W, Van Gelder P, Hartmann D, D'Hooge R, De Strooper B, Schymkowitz J, Rousseau F. Lipids revert inert Abeta amyloid fibrils to neurotoxic protofibrils that affect learning in mice. EMBO J. 2008 Jan 9;27(1):224-33. PubMed.
Shankar GM, Bloodgood BL, Townsend M, Walsh DM, Selkoe DJ, Sabatini BL. Natural oligomers of the Alzheimer amyloid-beta protein induce reversible synapse loss by modulating an NMDA-type glutamate receptor-dependent signaling pathway. J Neurosci. 2007 Mar 14;27(11):2866-75. PubMed.
Walsh DM, Selkoe DJ. A beta oligomers - a decade of discovery. J Neurochem. 2007 Jun;101(5):1172-84. PubMed.
View all comments by Barbara Calabrese�
I agree with Peter Lansbury. This is a beautiful piece of research, though the rapidity with which distinct plaques could be visualized is not surprising to those of us who have studied the deposition of beta-amyloid in near-physiological milieu in vitro. Neither should we be surprised that plaque formation was coincident with both an immune/inflammatory response and damage to the environment adjacent to the plaque.
I picked up my electronic copy of Nature early on the 7th and was able to present these results to medical students at 10.00 a.m. that morning. Congratulations are due to the authors for making simple what must have been extremely difficult to achieve.
View all comments by Chris ExleyAlzheimer Research Forum
This captures the extraordinarily rapid growth of Aβ plaques in real time using sophisticated longitudinal multiphoton microscopy. Microglial cells are “caught in the act” of activation and recruitment. The data make for compelling watching, almost like witnessing a crime.
What does this data suggest in terms of AD patients being treated with drugs to lower Aβ and to inhibit plaque formation? Do these new findings suggest that if drug treatment is discontinued, plaque growth and neurite dystrophy would recommence within days?
In addition, this study reminds me of a previous finding, incredible though it seemed at the time, that AD model mice demonstrated immediate cognitive improvement after passive anti-Aβ immunization (Dodart et al., 2002; Kotilinek et al., 2002). It would be informative if the in-vivo microscopy could be used after immunization to observe microglial activation and recruitment, since the technique has already been used to monitor neurite dystrophy following passive (or active) immunization (Brendza et al., 2005; Lombardo et al., 2003). The technique could be very useful to determine the relationship between microglial activation and neurite dystrophy in response to changing levels of plaque Aβ.
References:
Dodart JC, Bales KR, Gannon KS, Greene SJ, DeMattos RB, Mathis C, DeLong CA, Wu S, Wu X, Holtzman DM, Paul SM. Immunization reverses memory deficits without reducing brain Abeta burden in Alzheimer's disease model. Nat Neurosci. 2002 May;5(5):452-7. PubMed.
Kotilinek LA, Bacskai B, Westerman M, Kawarabayashi T, Younkin L, Hyman BT, Younkin S, Ashe KH. Reversible memory loss in a mouse transgenic model of Alzheimer's disease. J Neurosci. 2002 Aug 1;22(15):6331-5. PubMed.
Brendza RP, Bacskai BJ, Cirrito JR, Simmons KA, Skoch JM, Klunk WE, Mathis CA, Bales KR, Paul SM, Hyman BT, Holtzman DM. Anti-Abeta antibody treatment promotes the rapid recovery of amyloid-associated neuritic dystrophy in PDAPP transgenic mice. J Clin Invest. 2005 Feb;115(2):428-33. PubMed.
Lombardo JA, Stern EA, McLellan ME, Kajdasz ST, Hickey GA, Bacskai BJ, Hyman BT. Amyloid-beta antibody treatment leads to rapid normalization of plaque-induced neuritic alterations. J Neurosci. 2003 Nov 26;23(34):10879-83. PubMed.
View all comments by Gwendolyn WongIndiana University School of Medicine
Meyer-Luehmann and colleagues provide new insights into the temporal sequence of events surrounding amyloid plaque formation and the brain’s cellular responses to this formation. It is exciting to see that the rapid formation of plaques that had been predicted by previously published reports using in vitro techniques (Vitek et al., 1994; Jarrett et al., 1993) actually occurs in vivo. The concept of seeding by submicroscopic Aβ particles clearly remains an important mechanism for plaque formation and deposition.
Useful insights are also provided by visualization of the microglial response to the newly formed amyloid plaques. Microglia accumulate at the plaques, indicating the presence of activating/migration signals, most likely from Aβ. This, plus the microglial morphological changes, suggest that a pre-programmed response pattern, which is typical of macrophages involved in the innate immune response, has been initiated. However, it is clear from the visual data that the term “microglia activation” needs to be reconsidered and redefined. Although functional changes in the microglia were not measured, it is highly likely that a “proinflammatory” or classical activation sequence that is typically associated with severe tissue damage is limited either in time or amount. Other than the dystrophic neurites that could also be observed in non-plaque areas, there is no overt evidence of dying neurons in or around the plaques. While this lack of morphological evidence does not formally exclude the possibility that dying neurons are associated with plaques, the microglial response observed is consistent with what appears to be a “walling-off” response typical of an alternatively activated microglia.
Alternative activation is a response pattern of macrophages that is associated with fibrosis and tissue repair. Genes that typically participate in matrix remodeling and repair, such as arginase I, which governs proline/hydroxyproline production, and chitinase 3 like-2, are induced in this stage of microglial function. Inducible NOS (iNOS) activity is concomitantly lowered. We have shown that alternative activation genes are expressed in both mouse models of AD and in human brains with AD (Colton et al., 2006), confirming that microglia in chronic neurodegenerative diseases are likely to demonstrate significant functional heterogeneity that includes an alternative state.
The observed lack of amyloid plaque removal by microglia may be attributed to this altered functional state, where both protease production and phagocytic responses are likely to be different. It is clear that an additional stimulus is required to initiate microglial removal of amyloid. A series of studies on antibody therapy showed that anti-Aβ antibody administration, both intracranially and systemically, results in microglial activation and concomitant removal of compact amyloid plaques (Wilcock et al., 2003; 2004). Indeed, when microglial activation was inhibited by anti-inflammatory compounds or using F(ab’)2 fragment (thus avoiding Fc-receptor activation), no clearance of compact amyloid was seen (Wilcock et al., 2004). Application of intracranial injection of LPS, a well-known inducer of classical activation, was shown to reduce diffuse amyloid significantly but only temporarily, and this is consistent with the acute nature of LPS-mediated microglial stimulation (Dicarlo et al., 2001; Herber et al., 2004).
Together, these data suggest that microglia are ineffective in the removal of amyloid until a stimulus is available that alters their activation status from one of tissue remodeling to one of tissue defense.
References:
Vitek MP, Bhattacharya K, Glendening JM, Stopa E, Vlassara H, Bucala R, Manogue K, Cerami A. Advanced glycation end products contribute to amyloidosis in Alzheimer disease. Proc Natl Acad Sci U S A. 1994 May 24;91(11):4766-70. PubMed.
Jarrett JT, Berger EP, Lansbury PT. The carboxy terminus of the beta amyloid protein is critical for the seeding of amyloid formation: implications for the pathogenesis of Alzheimer's disease. Biochemistry. 1993 May 11;32(18):4693-7. PubMed.
Colton CA, Mott RT, Sharpe H, Xu Q, Van Nostrand WE, Vitek MP. Expression profiles for macrophage alternative activation genes in AD and in mouse models of AD. J Neuroinflammation. 2006;3:27. PubMed.
Wilcock DM, DiCarlo G, Henderson D, Jackson J, Clarke K, Ugen KE, Gordon MN, Morgan D. Intracranially administered anti-Abeta antibodies reduce beta-amyloid deposition by mechanisms both independent of and associated with microglial activation. J Neurosci. 2003 May 1;23(9):3745-51. PubMed.
Wilcock DM, Rojiani A, Rosenthal A, Levkowitz G, Subbarao S, Alamed J, Wilson D, Wilson N, Freeman MJ, Gordon MN, Morgan D. Passive amyloid immunotherapy clears amyloid and transiently activates microglia in a transgenic mouse model of amyloid deposition. J Neurosci. 2004 Jul 7;24(27):6144-51. PubMed.
Wilcock DM, Munireddy SK, Rosenthal A, Ugen KE, Gordon MN, Morgan D. Microglial activation facilitates Abeta plaque removal following intracranial anti-Abeta antibody administration. Neurobiol Dis. 2004 Feb;15(1):11-20. PubMed.
DiCarlo G, Wilcock D, Henderson D, Gordon M, Morgan D. Intrahippocampal LPS injections reduce Abeta load in APP+PS1 transgenic mice. Neurobiol Aging. 2001 Nov-Dec;22(6):1007-12. PubMed.
Herber DL, Roth LM, Wilson D, Wilson N, Mason JE, Morgan D, Gordon MN. Time-dependent reduction in Abeta levels after intracranial LPS administration in APP transgenic mice. Exp Neurol. 2004 Nov;190(1):245-53. PubMed.
Louisiana State University
Rapid Plaque Growth and Positive Cooperative Assembly
Amyloid-β peptides constitute an intriguing class of molecules that self-assemble into stable, ordered structures, and their formation is reminiscent of the natural phenomenon of positive cooperative assembly. In general, this cooperativity is regulated by an allosteric effect, so that interactive assemblies, once formed, support exponential rates of subsequent growth. In biology, this phenomenon is widely observed all the way from the atomic to the molecular level—from the cooperative binding of calcium ions regulating the intercellular adhesive actions of transmembrane cadherins (1) to the allosteric cooperativity of protein kinase A generated by nucleotide and substrate positioning (2).
Interestingly, allosteric cooperativity of ligand binding may be disrupted by single amino acid mutations, for example, the (Y204A) site change in protein kinase A, suggesting that relatively subtle changes in ligand topography abruptly attenuate the cooperativity mechanism. The addition to Meyer-Luehmann and colleagues’ innovative system of specific mutation-containing amyloid peptides or other interruptive molecules that do not support cooperative assembly may be an attractive pharmacological strategy to alter the kinetics of rapid plaque growth and the onset of Alzheimer neuropathology.
References:
Courjean O, Chevreux G, Perret E, Morel A, Sanglier S, Potier N, Engel J, Van Dorsselaer A, Feracci H. Modulation of E-cadherin monomer folding by cooperative binding of calcium ions. Biochemistry. 2008 Feb 26;47(8):2339-49. PubMed.
Masterson LR, Mascioni A, Traaseth NJ, Taylor SS, Veglia G. Allosteric cooperativity in protein kinase A. Proc Natl Acad Sci U S A. 2008 Jan 15;105(2):506-11. PubMed.
University of Maryland Baltimore
This is a fascinating paper, which I will be presenting in a journal club soon. I am sure there will be many answers from future studies using this imaging technique. But already it is interesting to see the rapid formation of amyloid plaques in vivo.
I wonder, however, could plaque formation happen even more rapidly in brain? The fluorescence dye used in this paper is a derivative of congo red, which may interfere with amyloid fibril formation. In this case, it is possible that the kinetics in this paper is still an underestimate. One thing that puzzles me, as a former Alzheimer researcher, is that environmental enrichment is reported to increase the number of amyloid plaques in the hippocampus of APPswe/PS1d9 mice (Jankowsky et al., 2003), while the same treatment also improves their learning performance (Jankowsky et al., 2005). How does that fit into the model?
Nevertheless, this paper has created new ground, and I assume that the authors have even more longitudinal imaging data in hand by now, hopefully for several months.
References:
Jankowsky JL, Xu G, Fromholt D, Gonzales V, Borchelt DR. Environmental enrichment exacerbates amyloid plaque formation in a transgenic mouse model of Alzheimer disease. J Neuropathol Exp Neurol. 2003 Dec;62(12):1220-7. PubMed.
Jankowsky JL, Melnikova T, Fadale DJ, Xu GM, Slunt HH, Gonzales V, Younkin LH, Younkin SG, Borchelt DR, Savonenko AV. Environmental enrichment mitigates cognitive deficits in a mouse model of Alzheimer's disease. J Neurosci. 2005 May 25;25(21):5217-24. PubMed.
VIB-KULeuven
Using sophisticated life imaging techniques, Meyer-Luehmann and colleagues looked at plaque formation in the mouse brain in real time. The paper shows exciting results demonstrating that plaque deposition is very fast and that many of the pathological changes associated with plaques do not precede, but follow deposition, suggesting a cause-consequence relationship. The overall picture emerging is that plaques rapidly crystallize out of solution. Obviously, as interesting as it is, this work does not address the question of the mechanism of toxicity, neither of what determines the dynamics and the rapid precipitation of plaques in the brain.
In our hands amyloid fibrils, as they are supposed to be present in amyloid plaques, display very little toxicity as such. Only when these mature fibrils become resolubilized, for instance, by lipids, do we generate what we called backward oligomers, which exert severe toxicity in neuronal culture and in brain of living animals (Martins and Kuperstein et al., 2008). There is also a recent study by Lesne and colleagues (2008) in plaque-bearing aged mice showing that memory impairment depends on soluble oligomers and not on the plaques. Thus, we remain with the question of whether the precipitated plaques seen by Meyer-Luehmann and colleagues directly cause toxicity, or whether around these plaques soluble oligomers or protofibrils are generated in dynamic equilibrium with the suddenly appearing plaques. If such an equilibrium exists, one would, however, have anticipated that plaques would appear and disappear, while these authors find that they are rather stable once they are formed. On the other hand, this exchange between soluble species and plaques may involve a limited number of deposited fibrils in the plaques that possibly does not change the structure of the plaque core once deposited, but is sufficient to produce toxic backward oligomers. Therefore, follow-up study of the presence of soluble oligomers, and of the dynamics of their appearance around the plaque, would be very interesting.
One of the main questions raised by several commentators is, If soluble oligomers are the major source of neurotoxicity, then why does neurodystrophy appear after the deposition of amyloid and not before? Conclusions cannot be made in this regard. There is the whole problem of kinetics and concentration-dependent factors that have to be taken into account. It could be that the threshold for toxicity is close to the threshold for amyloid precipitation, and that only close to the plaques sufficient oligomers are present to cause toxicity. The final neurodystrophy effect seen 5 days after the plaque “birthday” could also be simply the result of a relatively slow cumulative effect of protofibrils/oligomers present before deposition and maintained afterwards by “backward” toxic species released from this newborn plaque.
The question about stability of plaques as a function of time is also very intriguing. It would be informative to compare stability of fibrils in old and newborn plaques: the current study shows only the net result. In addition, it could indeed be that the microglia control the plaque size (Herber et al., 2007). In this regard, it becomes an interesting question to ask whether microglia are then protective, ensuring clearance of soluble toxic species, or whether they accelerate (backward) oligomer release.
References:
Martins IC, Kuperstein I, Wilkinson H, Maes E, Vanbrabant M, Jonckheere W, Van Gelder P, Hartmann D, D'Hooge R, De Strooper B, Schymkowitz J, Rousseau F. Lipids revert inert Abeta amyloid fibrils to neurotoxic protofibrils that affect learning in mice. EMBO J. 2008 Jan 9;27(1):224-33. PubMed.
Lesné S, Kotilinek L, Ashe KH. Plaque-bearing mice with reduced levels of oligomeric amyloid-beta assemblies have intact memory function. Neuroscience. 2008 Feb 6;151(3):745-9. PubMed.
Herber DL, Mercer M, Roth LM, Symmonds K, Maloney J, Wilson N, Freeman MJ, Morgan D, Gordon MN. Microglial activation is required for Abeta clearance after intracranial injection of lipopolysaccharide in APP transgenic mice. J Neuroimmune Pharmacol. 2007 Jun;2(2):222-31. PubMed.
View all comments by Inna KupersteinLund University
This landmark study provides many exciting new insights into the development of β amyloid plaques, and is a superb example of the importance of descriptive neuropathology research in elucidating Alzheimer disease (AD) pathogenesis. Using multiphoton microscopy to repeatedly image brain areas in transgenic mouse models of AD, the authors made several novel observations, including that plaques form within a day and remain stable in size, occur prior to microglial activation, and are not directly related to the vasculature. Another interesting new finding was that dystrophic neurites in plaque-free areas can appear and disappear.
The authors argue that their data indicate that plaques do not develop from dystrophic neurites, since plaques were not observed to form at sites of dystrophic neurites in plaque-free areas. Yet, looking closely at the brain cytoarchitecture prior to the appearance of a plaque, abundant neurites are evident, and with the limited resolution of multiphoton microscopy, early neuritic alterations could be missed spatially. They could also be missed temporally, as supplementary Figure 4 shows that neuritic dystrophy can be transient. In addition, compared to the many imaging sessions required to find emergence of new plaques (only 26 new plaques were found imaging 1,285 times at 238 sites in 14 mice), it is not specified how often the authors looked for the formation of plaques at sites of dystrophic neurites; only 10 examples are mentioned. Given how infrequently plaque formation was captured overall, following only 10 examples does not seem definitive.
The authors show that neuritic dystrophy follows plaque formation. However, they also observe that dystrophic neurites occur in plaque-free areas, indicating that extracellular plaques are not required for dystrophic neurite formation. Kumar-Singh points out in his comment that a higher power imaging method to view early β amyloid accumulation and dystrophic neurites at an ultrastructural level would be interesting. In fact, such electron microscopy studies have been done, reporting early intracellular β amyloid accumulation and even oligomerization within dystrophic neurites and synaptic compartments in both areas with and without plaques in AD transgenic mouse and human AD brain.
The Alzforum news story also notes: "whether a newly formed plaque changes neural activity...remains to be tackled." In our EM studies, we have consistently noted that even in the absence of plaques, intracellular Aβ accumulates prominently in neurites and synaptic compartments. Moreover, intracellular accumulation of Aβ is associated with marked ultrastructural pathology. Based on this ultrastructural pathology, it seems highly unlikely that these neurites and synapses would be capable of normal synaptic function. Both axonal and dendritic transport is also unlikely to be normal.
Before the current study is taken as proof that only extracellular β amyloid plays a role in the formation of plaques and neuritic dystrophy, one might want to keep an open mind for a role also of intraneuronal Aβ. An alternative scenario is that accumulation of intraneuronal Aβ both causes neuritic dystrophy and can be the nidus for extracellular plaque formation.
Make a Comment
To make a comment you must login or register.