Dementia à la Mold? Fungi May Lurk in Alzheimer’s Brains
Quick Links
Could infectious agents that enter the brain contribute in some way to neurodegenerative disease? This idea has been fermenting in recent years, and new data from researchers led by Luis Carrasco at the Autonomous University of Madrid add fuel to the brew. In the October 15 Scientific Reports, they report that fungi dot brains taken postmortem from people with Alzheimer’s, but not those from controls. The study does not address what the fungi might be doing, leaving it ambiguous whether the organisms exacerbate pathology or are merely opportunistic invaders. Nonetheless, researchers said the findings should stimulate efforts to understand the role of infectious agents in brain disease. “I believe this opens a new direction for research,” Carrasco told Alzforum.
The idea that infection might underlie Alzheimer’s pathology is not new. In 1910, Oskar Fischer, a contemporary of Alois Alzheimer, proposed that foreign bodies in the brain, possibly fungi, provoked inflammation and amyloid plaques (see Eikelenboom et al., 2006; Goedert, 2009; Mar 2009 conference news). “Alzheimer’s paper was a clinicopathological description of the disease, but Fischer presented the first hypothesis about its etiology and pathogenesis,” noted Piet Eikelenboom at Vrije University, Amsterdam (see also comment below).
While the idea never gained widespread acceptance, recent studies have sparked new interest in the concept. Researchers have reported, for example, that chlamydia pneumoniae and herpes simplex virus 1 infections can kick off Aβ plaque growth in mice, while a complex relationship has long been studied between HIV and dementia (see Jul 2002 conference news; Feb 2011 webinar; Oct 2004 conference news). In 2009, Robert Moir and Rudy Tanzi at Massachusetts General Hospital, Boston, made a case that Aβ is an antimicrobial that defends the body, and suggested that infection could trigger excess amyloid production and deposition (see Apr 2009 conference news; Apr 2015 conference news).
Few research groups have focused on fungi. However, Carrasco and colleagues previously reported finding fungal proteins in frozen brain tissue and cerebrospinal fluid from AD patients, but not in controls (see Alonso et al., 2014; Alonso et al., 2015). Immunostaining detected fungal cells inside frontal cortical neurons from Alzheimer’s patients (see Pisa et al., 2015).
Fungi in the AD Brain?
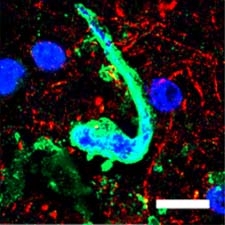
Structures in the entorhinal cortex of an AD patient contain fungal protein (green) and DNA (blue), suggesting they are fully fledged fungi. [Courtesy of Pisa et al., Scientific Reports.]
To determine how widespread fungi might be in the brain, first author Diana Pisa tested multiple brain regions from a single Alzheimer’s patient with several antibodies raised against fungal proteins. The antibodies bound a variety of shapes from the entorhinal cortex, hippocampus, frontal cortex, and cerebellum. These structures contained DNA, suggesting they were cells, and in some cases formed long fibrillar structures resembling the multicellular fungal threads known as hyphae. In addition, the structures appeared in cerebral blood vessels and in the choroid plexus that lines ventricles. The authors detected nothing similar in a postmortem brain from a normal healthy control.
To identify the species, the authors amplified fungal DNA from brain sections. They found six species of yeast, which grow as unicellular organisms, and four molds, which form hyphae. All were common fungi that typically live on skin or in soil and usually cause no health problems, but do occasionally infect people. Different species populated distinct brain regions in an eclectic mix.
How common are fungal infections in the brain? Entorhinal cortex and hippocampal samples from 10 additional AD brains all contained fungi, whereas none appeared in 10 additional controls of various ages. Fungi also dotted choroid plexus samples from three more AD patients, but not a control. “The fact that we find this in 100 percent of AD patients [tested] but no controls makes me optimistic that this is significant,” Carrasco noted.
Other researchers urged caution in interpreting the results. “The data need confirmation by skilled specialists,” wrote Kurt Jellinger of Vienna University School of Medicine in an email to Alzforum (see full comment below). “In our large [collection of] postmortem material of dementia and AD, we did not find any indications for fungal infections, although we did not use specific methods to detect fungal material in the brain.”
Brian Balin at the Philadelphia College of Osteopathic Medicine noted that all of the immunolabeling in this study was done with polyclonal antibodies, which may have poor specificity. Polyclonals raised against fungi might recognize polysaccharides, for example, which abound in AD brains. Alzheimer’s brains also contain a lot of fibrillar material that might resemble hyphae. Follow-up studies should use electron microscopy to zoom in on the structure of the labeled bodies and confirm that they represent hyphae and yeast cells, Balin suggested. Nonetheless, he found the paper intriguing for drawing more attention to the hypothesis that infection can be involved in neurodegenerative disease.
Other commenters agreed on the need for further study. Annemieke Rozemuller, a neuropathologist at VU University Medical Center, Amsterdam, noted that the paper does not address whether an active infection occurs around fungi, with infiltration of peripheral immune cells such as neutrophils and lymphocytes. Thus, it is unclear how much these organisms contribute to inflammation or pathology. She also would like to know at what stage fungi infiltrate the brain. Does this happen early in disease, leaving open the possibility that the organisms trigger pathology, or do the cells simply slip in late in disease through a weakened blood-brain barrier? It would be interesting to examine postmortem brains from people in early stages of cognitive impairment to address this, Rozemuller suggested.
Carrasco believes fungi might play a causative role in dementia. He noted two examples in the literature of people diagnosed with AD who were later treated for cryptococcal meningitis with antifungal medications, which reversed their dementia symptoms (see Ala et al., 2004; Hoffmann et al., 2009). Balin cautioned that treatment for any infectious agent should only be undertaken if there is evidence from blood or cerebrospinal fluid samples that the person has been exposed to that particular pathogen.—Madolyn Bowman Rogers
References
News Citations
- Prague: What Say You, Alois—Should It Be “Alzheimer-Fischer” Disease?
- Stockholm: Chlamydia Triggers Amyloid Plaques in Mice
- San Diego: HIV and AD—Save the Body, Lose the Mind?
- Prague: Aβ Rehabilitated as an Antimicrobial Protein?
- Could Adaptive Immunity Set the Brakes on Amyloid?
Webinar Citations
Paper Citations
- Eikelenboom P, Veerhuis R, Scheper W, Rozemuller AJ, Van Gool WA, Hoozemans JJ. The significance of neuroinflammation in understanding Alzheimer's disease. J Neural Transm. 2006 Nov;113(11):1685-95. PubMed.
- Goedert M. Oskar Fischer and the study of dementia. Brain. 2009 Apr;132(Pt 4):1102-11. PubMed.
- Alonso R, Pisa D, Marina AI, Morato E, Rábano A, Carrasco L. Fungal infection in patients with Alzheimer's disease. J Alzheimers Dis. 2014;41(1):301-11. PubMed.
- Alonso R, Pisa D, Rábano A, Rodal I, Carrasco L. Cerebrospinal Fluid from Alzheimer's Disease Patients Contains Fungal Proteins and DNA. J Alzheimers Dis. 2015;47(4):873-6. PubMed.
- Pisa D, Alonso R, Juarranz A, Rábano A, Carrasco L. Direct visualization of fungal infection in brains from patients with Alzheimer's disease. J Alzheimers Dis. 2015;43(2):613-24. PubMed.
- Ala TA, Doss RC, Sullivan CJ. Reversible dementia: a case of cryptococcal meningitis masquerading as Alzheimer's disease. J Alzheimers Dis. 2004 Oct;6(5):503-8. PubMed.
- Hoffmann M, Muniz J, Carroll E, De Villasante J. Cryptococcal meningitis misdiagnosed as Alzheimer's disease: complete neurological and cognitive recovery with treatment. J Alzheimers Dis. 2009;16(3):517-20. PubMed.
Further Reading
News
Webinars
Primary Papers
- Pisa D, Alonso R, Rábano A, Rodal I, Carrasco L. Different Brain Regions are Infected with Fungi in Alzheimer's Disease. Sci Rep. 2015 Oct 15;5:15015. PubMed.
Annotate
To make an annotation you must Login or Register.

Comments
Institute of Clinical Neurobiology
The importance of neuroinflammation and of disorders of the innate immune system in AD have been repeatedly documented in both animal models and human (autopsy) studies (McGeer and McGeer, 2013; Hensley, 2010; Baglio et al., 2013; Heneka et al., 2010; Wyss-Coray and Rogers, 2012; Boutajangout and Wisniewski, 2013; Zotova et al., 2010). Many investigators have suggested that infectious agents including herpes simplex 1 virus, other herpes viridae, and other pathogens, such as chlamydophila pneumoniae, cytomegalovirus, spirochetes, etc., constitute a risk factor or even a key causative factor in sporadic AD (Harris and Harris, 2015). Furthermore, the possibility that infectious agents may contribute to the progression of AD has been discussed (Honjo et al., 2009). The detection of fungal material in different brain regions in 11 of 11 AD brains but not in a single brain among 10 controls, together with the fungal proteins and RNA in CSF of AD patients detected by these researchers appears of interest. It indicates the necessity for further research in this area to confirm a potential causal effect of fungal infection in AD and suggests potentially treating AD with effective antifungal compounds.
However, it appears conjecture that these data indicating fungal infections of the brain tissue and vasculature as well as the CSF of AD patients have only been reported by a single group of scientists to date and, to the best of our knowledge, have not been confirmed by the large community of AD and related researchers. In our large postmortem material of dementia and AD, we did not find any indications for fungal infections, although we did not use specific methods to detect fungal material in the brain. It should be noted that degradation of Aβ peptide in cell cultures by mycoplasma contaminants has been reported and thus may represent a method of degradation of Aβ (Zhao et al., 2008).
The possibility that fungal infections may be related to AD pathology may be a challenge for future research in the etiology and pathogenesis of AD, but this latest data need confirmation by skilled specialists.
References:
McGeer PL, McGeer EG. The amyloid cascade-inflammatory hypothesis of Alzheimer disease: implications for therapy. Acta Neuropathol. 2013 Oct;126(4):479-97. Epub 2013 Sep 20 PubMed.
Hensley K. Neuroinflammation in Alzheimer's disease: mechanisms, pathologic consequences, and potential for therapeutic manipulation. J Alzheimers Dis. 2010;21(1):1-14. PubMed.
Baglio F, Saresella M, Preti MG, Cabinio M, Griffanti L, Marventano I, Piancone F, Calabrese E, Nemni R, Clerici M. Neuroinflammation and brain functional disconnection in Alzheimer's disease. Front Aging Neurosci. 2013;5:81. Epub 2013 Nov 25 PubMed.
Heneka MT, O'Banion MK, Terwel D, Kummer MP. Neuroinflammatory processes in Alzheimer's disease. J Neural Transm. 2010 Aug;117(8):919-47. PubMed.
Wyss-Coray T, Rogers J. Inflammation in Alzheimer disease-a brief review of the basic science and clinical literature. Cold Spring Harb Perspect Med. 2012 Jan;2(1):a006346. PubMed.
Boutajangout A, Wisniewski T. The innate immune system in Alzheimer's disease. Int J Cell Biol. 2013;2013:576383. Epub 2013 Oct 2 PubMed.
Zotova E, Nicoll JA, Kalaria R, Holmes C, Boche D. Inflammation in Alzheimer's disease: relevance to pathogenesis and therapy. Alzheimers Res Ther. 2010;2(1):1. PubMed.
Harris SA, Harris EA. Herpes Simplex Virus Type 1 and Other Pathogens are Key Causative Factors in Sporadic Alzheimer's Disease. J Alzheimers Dis. 2015;48(2):319-53. PubMed.
Honjo K, van Reekum R, Verhoeff NP. Alzheimer's disease and infection: do infectious agents contribute to progression of Alzheimer's disease?. Alzheimers Dement. 2009 Jul;5(4):348-60. PubMed.
Zhao H, Dreses-Werringloer U, Davies P, Marambaud P. Amyloid-beta peptide degradation in cell cultures by mycoplasma contaminants. BMC Res Notes. 2008;1:38. PubMed.
Vrije Universiteit
The idea that fungi could be the etiological agent of Alzheimer’s disease (AD) goes back to the earliest years of AD research. In the same year that Alzheimer described the case of Auguste D., Oskar Fischer published his paper about plaque formation. In this paper and a following one from 1910, Fischer stated that plaque formation was the result of an extracellular deposition of a peculiar foreign substance in the cortex that induced a local inflammatory reaction followed by a reactive response of the surrounding nerve fibrils (Fischer, 1907; Fischer, 1910). He stressed that the filamentous organization of this peculiar substance showed a strong similarity with fungi-like threads. Fischer supposed that this substance did not consist of dead matter but of live matter with a fungi-like organized structure. However, he could not observe around the plaques the morphological characteristics of an inflammatory response, and the complement binding studies for plaques were negative. In respect to the supposed infectious origin, he reported negative findings for microbial cell cultures. Fischer’s clinicopathological studies were well-known and widely debated in the first decades of the last century, but later they became neglected. Some years ago Michael Goedert published an article about Fischer’s work on dementia in the context of his life and time, and Gabrielle Strobel wrote about him in Alzforum (Goedert, 2009; Mar 2009 conference news).
About 70 years after Fischer’s publications, immunohistochemical studies revealed that plaques contain activated complement products and are associated with clusters of activated microglia. Subsequently it was found that fibrillar Aβ can activate the classical complement pathway. These findings indicate that Fischer was correct in his idea that plaques are the nidus of a chronic inflammatory response, but not in his opinion that this response is induced by micro-organisms (Eikelenboom et al., 2006). AD is now considered as an auto-inflammatory disease. Recently there has been renewed interest in the role of micro-organisms as an etiological agent of AD (Welling et al., 2015). Several studies have shown an association between infection burden and AD. Furthermore, experimental studies suggest that Aβ can be considered a “host defense peptide” with antimicrobial activity. These findings suggest that Fischer’s “peculiar foreign substance,” while not infectious, could be the result of an antimicrobial response against infections. It seems that in science, some ideas, like old soldiers, never die.
References:
Eikelenboom P, Veerhuis R, Scheper W, Rozemuller AJ, Van Gool WA, Hoozemans JJ. The significance of neuroinflammation in understanding Alzheimer's disease. J Neural Transm. 2006 Nov;113(11):1685-95. PubMed.
Fischer O. Miliare Nekrosen mit drusigen Wucherungen der Neurofibrillen, eine regelmässige Veränderung der Hirnrinde bei seniler Demenz. Monatsschr Psychiat Neurol. 1907;22:361-72.
Fischer O. Die presbyophrene Demenz, deren anatomische Grundlage und klinische Abgrenzung. Z ges Neurol Psychiat. 1907;3:371-471.
Goedert M. Oskar Fischer and the study of dementia. Brain. 2009 Apr;132(Pt 4):1102-11. PubMed.
Welling MM, Nabuurs RJ, van der Weerd L. Potential role of antimicrobial peptides in the early onset of Alzheimer's disease. Alzheimers Dement. 2014 Mar 15; PubMed.
Victoria University
This study keeps alive the flame that may illuminate the underlying microbial involvement in neurodegenerative diseases (NDs) afflicting humans. The tantalizing evidence of the presence of fungi in the Alzheimer’s disease brain, but not controls, does point toward a role of infectious agents that enter the brain and contribute in some way to the development of NDs, in this case AD. The study also raises an important question about whether the classical human NDs are largely non-classical in nature. How widespread and consistent this involvement is remains to be determined.
Although this idea has been brewing for decades, with a number of anecdotal reports hinting at the involvement of viral and now fungal organisms in human NDs, the advances in high-throughput genomics and proteomics have provided further clues to the involvement of microbes. Including this study, other studies have also not addressed what the microbes might be doing in the CNS of the aging brain, raising the question of whether these organisms exacerbate pathology or are merely opportunistic invaders partly due to the age of the immune system.
In this context, it is important to mention that both genomic and proteomic studies by Zhou et al. strongly suggest intrinsic involvement of the immune pathways in human NDs, where we least expect the expression of these pathways. This solidifies the idea of possible microbial involvement in human NDs. Although a large majority of studies do not support involvement of pathogenic etiology in classical NDs, a number of emerging studies show support for possible association of viruses with classical neurodegenerative diseases in humans. Viruses induce alterations and degeneration of neurons both directly and indirectly. Their ability to attack the host immune system and regions of the nervous tissue implies that they can interfere with the same pathways involved in classical NDs in humans. Many similarities between classical NDs and virus-mediated, i.e. non-classical, neurodegeneration have been shown at the anatomic, subcellular, genomic, and proteomic levels suggesting that viruses can explain neurodegenerative disorders mechanistically (Zhou et al., 2013). If fungal invasion in AD is true, both fungi and viruses can guide us to unveil these pathways in human NDs, which will further stimulate the birth of new concepts in the biological research needed for gaining deeper insights into the treatment of human NDs and delineate mechanisms underlying neurodegeneration in humans.
Recently, Zhou et al. (2010) showed the first evidence of overlaps between HIV-associated dementia (HAD) and non-viral neurodegenerative diseases through proteomic analysis of the frontal cortex from HIV-positive patients with and without dementia. The large majority of identified proteins were represented in mitochondrial energy metabolic and signal transduction pathways. More than 90 percent of the protein candidates were common to both HAD and other non-viral neurodegenerative diseases, such as Alzheimer's disease, lending further credence to the current findings shown by Carrasco’s group in the context of fungal invasion of the CNS in the aging brain with AD.
More recently, Zhou et al. asked why ND-related pathways are over-represented in primary HIV-infected peripheral blood mononuclear cells in patients without dementia or HIV-related AD and Parkinson’s disease, and they provided the first genome-wide perspective through cell-tagging analysis (Zhou et al., 2012). They suggest that the genome-wide representation of neurodegenerative disease-related pathways in PBMCs could possibly be a subcellular manifestation of neurologic interference by HIV. Their analysis showed the large majority of genes tagged with cells of monocyte and macrophage lineage, which are implicated in neuronal dysfunction in both viral and non-viral neurodegenerative diseases. Together, these findings suggested that the genomic interference of HIV with neurodegenerative pathways is not by chance, but may be an early sign of HIV-mediated manifestation of neurologic disease. Moreover, the study by Zhou and the current study by Carrsaco’s group signify the utility of data in predicting possible early events in neurologic deterioration in humans.
Brian Balin noted that all of the immunolabeling in this study was done with polyclonal antibodies, which may have poor specificity. The result definitely warrants further confirmation. Balin made a very valid point. One needs proteomic studies to see if fungal proteins are there, in addition to ultra-structural studies using transmission immune-electron microscopy with monoclonals. Studies such as this one are needed to make the point that infection can be involved in neurodegenerative disease, because in the aging immune system the infectious and/or opportunistic modalities are more likely to cause damage. That is why it has been difficult to find active infection in AD brains by many studies that suggest microbial involvement in human NDs. Annemieke Rozemuller rightly questions active infection with fungi, but if we can determine at what stage fungi infiltrate the brain and what happens to it at different stages, then we may be able to determine how the progressive damage results up to the manifestation of AD.
Overall, I find the study tantalizing. It raises a pertinent and obscure question about the pathology and etiology of AD that has eluded us to date. Studies along the lines of Zhou et al.’s are needed to holistically understand the molecular basis of the neurodegenerative diseases that afflict us.
References:
Zhou L, Miranda-Saksena M, Saksena NK. Viruses and neurodegeneration. Virol J. 2013 May 31;10:172. PubMed.
Zhou L, Diefenbach E, Crossett B, Tran SL, Ng T, Rizos H, Rua R, Wang B, Kapur A, Gandhi K, Brew BJ, Saksena NK. First evidence of overlaps between HIV-Associated Dementia (HAD) and non-viral neurodegenerative diseases: proteomic analysis of the frontal cortex from HIV+ patients with and without dementia. Mol Neurodegener. 2010;5:27. PubMed.
Zhou L, Conceicao V, Gupta P, Saksena NK. Why are the neurodegenerative disease-related pathways overrepresented in primary HIV-infected peripheral blood mononuclear cells: a genome-wide perspective. Virol J. 2012;9:308. PubMed.
Quietmind Foundation
The researchers are to be commended for realizing the emerging role of pathogens in Alzheimer's disease. We submitted an abstract on this topic for the Society for Neuroscience Annual Meeting in 2012 based on the work of Alan MacDonald, Nias Mattsson et al., Geeta Ramesh and colleagues, and Judith Miklossy's group on Borrelia and periodontal treponema pathogens. Transitional therapy with antibiotics and with moderate magnetic fields demonstrated temporary symptom improvement in a small pilot study.
See also:
Nichols TW, MacDonald AB (2012). Emerging role of pathogens in Alzheimer's and moderate magnetic field therapy:DC Emf 0.5 tesla ;SFN poster, July 17,9:58:52 AM
References:
MacDonald AB. Plaques of Alzheimer's disease originate from cysts of Borrelia burgdorferi, the Lyme disease spirochete. Med Hypotheses. 2006;67(3):592-600. Epub 2006 May 3 PubMed.
MacDonald AB. Alzheimer's disease Braak Stage progressions: reexamined and redefined as Borrelia infection transmission through neural circuits. Med Hypotheses. 2007;68(5):1059-64. PubMed.
MacDonald AB. Alzheimer's neuroborreliosis with trans-synaptic spread of infection and neurofibrillary tangles derived from intraneuronal spirochetes. Med Hypotheses. 2007;68(4):822-5. PubMed.
Miklossy J. Alzheimer's disease - a neurospirochetosis. Analysis of the evidence following Koch's and Hill's criteria. J Neuroinflammation. 2011;8:90. PubMed.
Miklossy J, Khalili K, Gern L, Ericson RL, Darekar P, Bolle L, Hurlimann J, Paster BJ. Borrelia burgdorferi persists in the brain in chronic lyme neuroborreliosis and may be associated with Alzheimer disease. J Alzheimers Dis. 2004 Dec;6(6):639-49; discussion 673-81. PubMed.
Mattsson N, Bremell D, Anckarsäter R, Blennow K, Anckarsäter H, Zetterberg H, Hagberg L. Neuroinflammation in Lyme neuroborreliosis affects amyloid metabolism. BMC Neurol. 2010;10:51. PubMed.
Universidad Autónoma de Madrid
In our opinion, we have provided compelling evidence for fungal infection in CNS of all AD patients analyzed. However, to distinguish between two possibilities, i.e., that fungal infection is the cause or a consequence of AD, clinical trials using antifungal compounds should be carried out. In support of the concept that fungal infection may be causing AD, here are several considerations:
These observations point to the possibility that fungal infection provokes AD. Thus, pharmaceutical companies in collaboration with hospitals now have scientific grounds on which to plan a pilot clinical trial.
There is also the possibility that other microbes can participate in the pathology of AD. As indicated by several commentators, some viruses, particularly of the herpervirus group, or some bacteria, can play a part in AD. My own background is in virology (see my publications), and we are investigating this possibility.
I am looking forward to other scientists in other countries, who have access to brain banks, being interested in addressing our recent results. If results by other groups are positive, then clinical trials could be performed. My work has provided a first step in a new and thus far unsuspected direction to pursue research on AD, i.e., that its etiology is due to disseminated and mixed fungal infections. The fact that the fungal species present in each patient varies is consistent with the fact that the evolution and severity of symptoms in each AD patient is also different.
As to the dogma of amyloid-tau as the cause of AD, a number of recent results do not support it. For instance, several compounds have been developed by pharmaceutical companies that interfere with formation of amyloid plaques or with tau tangles, but after treating AD patients with these compounds, the clinical symptoms were not modified.
Apart from AD, a number of other chronic diseases progress slowly, including other neurodegenerative diseases that have also signs of inflammation. Thus, we can speculate that perhaps other human diseases could be of fungal origin. In this sense, it will be helpful to improve diagnosis assays to conclude the presence of fungal infections in these patients.
References:
Soscia SJ, Kirby JE, Washicosky KJ, Tucker SM, Ingelsson M, Hyman B, Burton MA, Goldstein LE, Duong S, Tanzi RE, Moir RD. The Alzheimer's disease-associated amyloid beta-protein is an antimicrobial peptide. PLoS One. 2010 Mar 3;5(3):e9505. PubMed.
Massachusetts General Hospital & Harvard Medical School
Massachusetts General Hospital
Investigations into possible roles for infection and associated immune response in AD etiology have a long history, but have gained increasing attention and impetus in recent years. In 2014, more than 80 publications were cited on PubMed supporting increased CNS infection in AD. Diverse and overwhelming epidemiological and experimental data now support increased CNS infection with AD. However, claims that infection may drive the hallmark pathologies in AD, amyloidosis and neurofibrillary tangles, are most often met with skepticism, and support for pathogens as etiological factors is limited to a small subset of AD researchers.
Historically, concerns have been voiced about what conclusions can be drawn from data showing infectious agents in AD brain, such as those of Pisa et al. These are concerns common to many discussions of studies linking pathogens to AD etiology. At least three arguments typically arise in various forms against the conclusion that increased CNS infections in AD implies that pathogens are etiological factors for the disease:
These longstanding concerns have stymied the serious consideration of infection as an etiological factor for AD. However, the new data from Pisa et al. once again raise the issue.
Much of the historical skepticism for clinical pathogens as etiological factors for AD comes from the leading model of β-amyloidogenesis. Aβ is most often characterized as a functionless catabolic byproduct of APP. The activities of Aβ peptides are considered intrinsically abnormal, particularly the propensity for self-association. The view that all Aβ activities are pathological was a reasonable hypothesis following the peptide's discovery. The contention that Aβ is an incidental product of catabolism, and by extension that its activities serve no physiological function, has persisted almost unchallenged for two decades. This is in spite of evidence showing that Aβ is found unchanged in most vertebrate species across at least 400 million years of phylogenetic history (humans share Aβ42 sequences with coelacanths, an ancient fish taxon; see Luna et al., 2013). The remarkable conservation of the Aβ sequence and associated activities suggests that the peptide mediates an important normal physiological pathway.
We have previously proposed that Aβ plays a role in innate immunity as an antimicrobial peptide (AMP) (Soscia et al., 2010). We believe our emerging model of a protective antimicrobial role for Aβ may be useful in addressing at least the latter two common arguments raised against infection-driven AD pathology. In 2010, we published the first report that Aβ functions as an antimicrobial peptide (Soscia et al., 2010). In vitro, Aβ exerts antimicrobial activities equivalent in potency and spectrum to classical AMPs, the protective actions of which are recognized as critically important for normal human immunity.
We currently have a manuscript under review validating Aβ's antimicrobial actions in vivo in several different disease models (mouse, Drosophila, C. elegans, and neuronal cultures). Our data suggest that β-amyloid deposition is part of a normally protective innate immune antimicrobial pathway. Aβ expression in these models protects against the fungus Candida albicans and against Salmonella bacterium in various experimental models. Most importantly, the protective actions were mediated by the generation of β-amyloid, which acts to inhibit infection. The clinical pathogens tested were also able to rapidly seed the formation of β-amyloid. This addresses the second argument, and identifies a direct pathway by which clinical microbial pathogens may accelerate amyloidosis in the brain. In this model, increased Aβ deposition is considered part of a general response mounted by the innate immune system to a CNS infection.
Aβ inhibits fungi and bacteria, plus three independent studies have shown activity against viruses (White et al., 2014; Bourgade et al., 2015). Thus, Aβ fibrillization is not specific for an individual microbial species but can be generated in response to a broad range of pathogens in AD brain. This addresses the third argument, and may explain why a single pathogen is not overwhelmingly associated with AD. This is also consistent with the Pisa et al. data that show a range of fungal species in AD brain.
Independent evidence from a variety of approaches will be needed to answer the first and key question of whether infection is a consequence or an initiator of AD pathology. Our model of a normal protective antimicrobial role for Aβ and β-amyloid agrees with a view in which clinical pathogens drive β-amyloidosis (with precedents from several other AMPs and associated amyloidoses).
So-called sterile inflammatory diseases are also mediated through dysregulation of innate immunity; AD likely shares this etiology, as well. However, the convergence of data showing infection is part of AD pathology and an emerging antimicrobial role for Aβ that provokes the accumulation of β-amyloid is highly provocative. We have come to call this new model of AD etiology the “antimicrobial defense hypothesis.” Pisa et al. provide further evidence of the pressing need to explore these new models, and for a comprehensive and balanced reassessment of the ideas underpinning current views of AD as the consequence of the stochastic misbehaviors of a purportedly purposeless peptide.
References:
Pisa D, Alonso R, Rábano A, Rodal I, Carrasco L. Different Brain Regions are Infected with Fungi in Alzheimer's Disease. Sci Rep. 2015 Oct 15;5:15015. PubMed.
Luna S, Cameron DJ, Ethell DW. Amyloid-β and APP Deficiencies Cause Severe Cerebrovascular Defects: Important Work for an Old Villain. PLoS One. 2013;8(9):e75052. PubMed.
Soscia SJ, Kirby JE, Washicosky KJ, Tucker SM, Ingelsson M, Hyman B, Burton MA, Goldstein LE, Duong S, Tanzi RE, Moir RD. The Alzheimer's disease-associated amyloid beta-protein is an antimicrobial peptide. PLoS One. 2010 Mar 3;5(3):e9505. PubMed.
White MR, Kandel R, Tripathi S, Condon D, Qi L, Taubenberger J, Hartshorn KL. Alzheimer's associated β-amyloid protein inhibits influenza A virus and modulates viral interactions with phagocytes. PLoS One. 2014;9(7):e101364. Epub 2014 Jul 2 PubMed.
Bourgade K, Garneau H, Giroux G, Le Page AY, Bocti C, Dupuis G, Frost EH, Fülöp T Jr. β-Amyloid peptides display protective activity against the human Alzheimer's disease-associated herpes simplex virus-1. Biogerontology. 2015 Feb;16(1):85-98. Epub 2014 Nov 7 PubMed.
RMIT University
It is pleasing to see that the pathogen hypothesis of Alzheimer’s disease is finally receiving serious attention. However, the concept that Aβ plays a role in innate immunity as an antimicrobial peptide significantly predates Soscia et al. (2010) or Robert Moir and Rudy Tanzi (2009). The concept was postulated in 2002, in an open peer commentary, published in Neurobiology of Aging (Robinson and Bishop, 2002). In that paper we argued that the amyloid cascade hypothesis was inconsistent with a wide range of experimental observations and therefore was likely to be wrong. We noted that the widespread occurrence of Aβ in healthy individuals strongly suggests that Aβ plays a natural physiological role, one that is most probably protective. We postulated that "Aβ may have a broader role as a general chelator and flocculant of potentially toxic agents that are dissolved in the extracellular fluid. In addition to metal ions, this would include bacteria and viruses, proteins, and neuroactive molecules that have been inadvertently released into the extracellular fluid." We termed this the "Bioflocculant Hypothesis" of Aβ. In a companion paper (Robinson and Bishop, 2002), we reiterated that "The bioflocculant hypothesis supports a beneficial role for Aβ peptide, but the focus of the hypothesis is on the capacity of Aβ to bind and immobilize a wide variety of neurotoxic agents. The neutralization and removal of these agents from the extracellular space is the primary function of Aβ … agents that are snared by Aβ include most metal ions (not just copper and zinc), many proteins and macromolecules (such as those released during the inflammatory cascade), as well as pathogens (such as bacteria and viruses)." Once bound and taken out of solution, we envisaged that these pathogenic agents could be phagocytosed and cleared by microglia and macrophages. We noted that the Bioflocculant Hypothesis makes a range of predictions that are readily testable. This recent data provided by Pisa et al. (2015) and the additional observations summarized by Robert Moir and Rudy Tanzi in the accompanying commentary, go a long way to providing support for the Bioflocculant Hypothesis.
References:
Soscia SJ, Kirby JE, Washicosky KJ, Tucker SM, Ingelsson M, Hyman B, Burton MA, Goldstein LE, Duong S, Tanzi RE, Moir RD. The Alzheimer's disease-associated amyloid beta-protein is an antimicrobial peptide. PLoS One. 2010 Mar 3;5(3):e9505. PubMed.
Robinson SR, Bishop GM. Abeta as a bioflocculant: implications for the amyloid hypothesis of Alzheimer's disease. Neurobiol Aging. 2002 Nov-Dec;23(6):1051-72. PubMed.
Bishop GM, Robinson SR. The amyloid hypothesis: let sleeping dogmas lie?. Neurobiol Aging. 2002 Nov-Dec;23(6):1101-5. PubMed.
Universities of Manchester and Oxford
Steve Robinson's comment that it is good to see the concept of infectious agents' involvement in AD now being taken seriously is so apposite—as is the mention of his pioneering hypothesis 14 years ago on Aβ's protective action. The fungal study by Pisa et al. is intriguing, but obviously it is essential to replicate the data in other labs, and to find if the fungi are active, and if their presence in the brain is not merely a consequence of the disease. Hopefully, those working on the topic will not face the same extreme hurdles in obtaining grants and having papers accepted as have researchers in the past who studied Chlamydia pneumoniae, Borrelia, and herpes simplex virus type 1 (HSV1) in relation to AD. These difficulties occurred despite good evidence that the microbes play a major role in AD—(certainly not "merely opportunistic invaders"), e.g., in the case of HSV1, that it resides in elderly brains (Jamieson et al., 1991), is active there (Wozniak et al., 2005), and confers a major risk of AD when in the brains of APOE-e4 carriers (Itzhaki et al., 1997). Further, HSV1 causes accumulation of Aβ and AD-like tau in cell cultures (as do the two types of bacteria), and HSV1 DNA is located specifically in AD amyloid plaques (see reviews: Wozniak and Itzhaki, 2012; Itzhaki, 2014).
Considering HSV1, the number of papers supporting its role in AD has steadily increased: In 2014 there were some 37 supportive papers by groups other than mine (Itzhaki, 2014); now there are about 50. To explain the frequent and often virulent (though wholly unsubstantiated) opposition to the HSV1-AD concepts, I suggested that several basic concepts are often not understood: that microbes can cause chronic as well as acute diseases; that they can remain in the body lifelong, probably latent but reactivating during stress, immunosuppression, etc.; and that infected does not necessarily mean affected, i.e., some infected people might be asymptomatic “controls.” Appreciating these facts would surely lead to provision of funds (after years of refusals) for a clinical trial of an antiviral to treat AD—especially as current antivirals are very effective and safe—in the hope of slowing or even stopping disease progression.
References:
Jamieson GA, Maitland NJ, Wilcock GK, Craske J, Itzhaki RF. Latent herpes simplex virus type 1 in normal and Alzheimer's disease brains. J Med Virol. 1991 Apr;33(4):224-7. PubMed.
Wozniak MA, Shipley SJ, Combrinck M, Wilcock GK, Itzhaki RF. Productive herpes simplex virus in brain of elderly normal subjects and Alzheimer's disease patients. J Med Virol. 2005 Feb;75(2):300-6. PubMed.
Itzhaki RF, Wozniak MA. Could antivirals be used to treat Alzheimer's disease?. Future Microbiol. 2012 Mar;7(3):307-9. PubMed.
Itzhaki RF. Herpes simplex virus type 1 and Alzheimer's disease: increasing evidence for a major role of the virus. Front Aging Neurosci. 2014;6:202. Epub 2014 Aug 11 PubMed.
Itzhaki RF, Lin WR, Shang D, Wilcock GK, Faragher B, Jamieson GA. Herpes simplex virus type 1 in brain and risk of Alzheimer's disease. Lancet. 1997 Jan 25;349(9047):241-4. PubMed.
University of Edinburgh
The finding of Carrasco and colleagues (Pisa et al., 2015) of fungal species in Alzheimer disease (AD) brains is of great interest. This follows on from earlier reports of herpes simplex virus (Itzhaki and Wozniak, 2008) and bacteria including spirochetes (Miklossy, 2015) in AD brain tissue.
A wider perspective is that we are all exposed to multiple organisms that—given an opportunity—proliferate. In addition, the immune system undoubtedly declines with age, and therefore the presence of pathogens in the aging brain might not be so surprising.
Infection could be a general feature of age-related disease. In addition to AD, intermittent reports have linked brain infection to Parkinson's disease and depression. Tissue pathogens have been reported in conditions ranging from arthritis to atherosclerosis to diabetes.
The central issue is whether infection contributes to these diseases, or is a bystander.
Aβ peptide provides a clue. Once regarded as the culprit in AD, Aβ peptide is increasingly recognized to have antimicrobial properties (Soscia et al., 2010), lending support to the “antimicrobial defense hypothesis” of Moir and Tanzi. Indeed, Aβ deposition, a hallmark of AD, is also reported in cases of brain infection with HIV (Esiri et al., 1998; Green et al., 2005) and herpesvirus (Bearer et al., 2013). Looking more widely, arterial Aβ deposition is recorded in atherosclerosis, another age-related condition in which infection is implicated (Lathe et al., 2014, for review).
The presence of Aβ therefore most likely reflects an ongoing state of microbial proliferation and/or immune system activation. However, it falls short of defining whether the proliferation of infectious agents causes neuronal loss in AD.
In some ways the experiment has already been done! Brain HIV infection in younger people causes both Aβ deposition and HIV dementia (Navia et al., 1986).
Two questions come to the fore. First, does the immune system decline naturally with aging—or do the infectious agents such as CMV themselves contrive this outcome (e.g., Pawelec et al., 2004)? Indeed, CMV infection was specifically noted as an ancillary to HIV dementia (Navia et al., 1986). Second, if we could hold back these pathogens (using antivirals, antifungals, or vaccination), particularly those that distort the immune system (e.g., CMV), would we also hold back AD? Trials to address this promising new area of AD research are certainly warranted.
References:
Bearer EL, Woltjer R, Donanue JE, Kilpatrick K. Herpes encephalitis and Abeta plaques. . FASEB J. 2013 Apr;27(1 Suppl):873.16.
Esiri MM. Viruses and Alzheimer's disease. J Neurol Neurosurg Psychiatry. 1982 Aug;45(8):759-60. PubMed.
Green DA, Masliah E, Vinters HV, Beizai P, Moore DJ, Achim CL. Brain deposition of beta-amyloid is a common pathologic feature in HIV positive patients. AIDS. 2005 Mar 4;19(4):407-11. PubMed.
Itzhaki RF, Wozniak MA. Herpes simplex virus type 1 in Alzheimer's disease: the enemy within. J Alzheimers Dis. 2008 May;13(4):393-405. PubMed.
Lathe R, Sapronova A, Kotelevtsev Y. Atherosclerosis and Alzheimer - diseases with a common cause? Inflammation, oxysterols, vasculature. BMC Geriatr. 2014 Mar 21;14:36. PubMed.
Miklossy J. Historic evidence to support a causal relationship between spirochetal infections and Alzheimer's disease. Front Aging Neurosci. 2015;7:46. Epub 2015 Apr 16 PubMed.
Navia BA, Cho ES, Petito CK, Price RW. The AIDS dementia complex: II. Neuropathology. Ann Neurol. 1986 Jun;19(6):525-35. PubMed.
Pawelec G, Akbar A, Caruso C, Effros R, Grubeck-Loebenstein B, Wikby A. Is immunosenescence infectious?. Trends Immunol. 2004 Aug;25(8):406-10. PubMed.
Pisa D, Alonso R, Juarranz A, Rábano A, Carrasco L. Direct visualization of fungal infection in brains from patients with Alzheimer's disease. J Alzheimers Dis. 2015;43(2):613-24. PubMed.
Soscia SJ, Kirby JE, Washicosky KJ, Tucker SM, Ingelsson M, Hyman B, Burton MA, Goldstein LE, Duong S, Tanzi RE, Moir RD. The Alzheimer's disease-associated amyloid beta-protein is an antimicrobial peptide. PLoS One. 2010 Mar 3;5(3):e9505. PubMed.
New York Institute of Medical Research
Actually, what Oskar Fischer, the co-discoverer of Alzheimer’s disease, saw was Streptothrix, a germ with both bacterial and fungal properties often confused with tuberculosis. The disease actinomycosis was at one time referred to interchangeably with its older bacterial name, the “Streptotriches” (the plural form of Streptothrix). Fischer used such older nomenclature in describing certain forms he saw under his microscope.
Regarding the thick, black, club-shaped “drüsen” in Fischer's 1907 drawing of senile plaque―at the time, it was widely acknowledged that such drüsen could result from either infection with Streptothrix, now known as actinomycosis (aktinomycesdruse), a rare disease in humans, or tuberculosis, a disease that by 1882, as Alzheimer prepared to leave for Berlin for his medical education, was understood to be far and away the leading cause of infectious death in Europe.
And just 10 years before Fischer found Actinomycosis-like forms in Alzheimer’s cerebral plaque, Babèş and immunologist Levaditi reported in “On the Actinomycotic Shape of the Tuberculous Bacilli” that typical Actinomyces-like clusters (drüsen) with clubs appeared in the tissue of rabbits inoculated with tubercle bacilli beneath the dura mater of their brains. Once introduced into the brain this way, reported Babes, TB bacilli not only branched out like the Actinomycosis such as Streptothrix, but they developed rosettes that were identical to the “drüsen” that Fischer spotted in Alzheimer’s plaque.
References:
O. Fischer, “Miliary Necrosis with Nodular Proliferation of the Neurofibrils: A Common Change of the Cerebral Cortex in Senile Dementia,” Monatsschrift fur Psychiatrie und Neurologie, vol. XXII, Th. Ziehen (ed). (Berlin: Karger, 1907), 361–72; In The Early Story of Alzheimer’s Disease, edited by Katherine Bick, Luigi Amaducci, and Giancarlo Pepeu (Padova: Liviana Press, 1987), 5–18.
V. Babes and C. et Levaditi, “On the Actinomycotic Shape of the Tuberculosis Bacilli” (“Sur la Forme Actinomycosique du Bacilli de la Tuberculosis”), In Arch. of Med. Exp. et D’anat, part 2, 9, no. 6 (1897): 1041–8.
L. Broxmeyer, “Alzheimer’s Disease―How Its Bacterial Cause was Found and then Discarded.” Create Space Independent Platform, 2016. 165 pp
Make a Comment
To make a comment you must login or register.