Metabolomics: Metabolism and Omics in Alzheimer’s Disease
Quick Links
Metabolomics holds the promise of giant metabolite screens, leading to a bounty of clues to Alzheimer’s disease (see Part 1). Alzheimer’s researchers are certainly familiar with big science; the Alzheimer’s Disease Neuroimaging Initiative (ADNI) is entering its seventh year. Omics has played no small part in ADNI; indeed, the Initiative recently released data from a proteomics study. Metabolism has long been suspected in Alzheimer’s, with certain variants of the cholesterol-packer ApoE conferring risk, and abnormalities in glucose use showing up early in the brains of people at risk for AD. Researchers have conducted several pilot studies in metabolomics for Alzheimer’s and other neurodegenerative diseases (see Part 4). However, the methods of metabolomics (see Part 2) are not yet mature enough to partner with a large-scale study such as ADNI, said Bill Potter of Philadelphia, who chairs the Initiative’s proteomics working group.
Omics experiments require carefully standardized methods, Potter told ARF. “It has taken us much longer to agree on a reliable measure for proteomics than we thought it would,” he said. The proteomics data released by ADNI in November of 2010 include plasma analysis for 190 proteins already known to be related to AD or other diseases. Of course, some variation that appears to relate to AD or mild cognitive impairment (MCI) could also be due to age or gender. Potter is awaiting better methods before ADNI will prospect for unknown proteins. Similarly, he would like to see more groups validate metabolomics methods. “Metabolomics has huge downstream potential,” he said, but “there certainly is not yet agreement that the method is mature enough to make ADNI samples available.”
Although it is too soon to run such a large metabolomics study, scientists are pursuing several pilot projects. In an upcoming paper, Rima Kaddurah-Daouk of Duke University in Durham, North Carolina, and colleagues intend to report on metabolomic profiles of the cerebrospinal fluid (CSF) of 120 people with AD or MCI. They have measured a few hundred chemicals, Kaddurah-Daouk told ARF, and are searching for links with plaques, tangles, and disease severity. “It is going to be a nice, big matrix of the correlations,” she said.
That study is a follow-up on a previous, smaller project with postmortem material (Kaddurah-Daouk et al., 2010). The researchers measured 33 known metabolites in postmortem CSF samples from 15 people confirmed to have had Alzheimer’s disease and 15 non-demented controls. Norepinephrine levels were low in the AD subjects, and several other metabolic pathways showed differences as well. Of course, postmortem samples only reflect the final stages of disease; the new study should provide data on earlier phases.
Kaddurah-Daouk also expects soon to publish a study focused on lipids in AD. The lipidome can separate ApoE4 carriers from non-carriers, she told ARF. The scientists are still verifying their unpublished findings, but the work suggests that a given ApoE genotype comes with a unique lipidome signature.
In another preliminary study, Cristina Legido-Quigley of King’s College London, U.K., used liquid chromatography and mass spectrometry to analyze plasma from 16 people with AD, 12 with mild cognitive impairment (MCI), and 10 healthy controls (Greenberg et al., 2009). Many metabolites that show up in a screen such as this tend to be unknown. Even so, the researchers were able to identify three bile acids that were increased in MCI and AD samples, though the effect did not reach statistical significance. Glycocholic acid, glycodeoxycholic acid, and glycochenodeoxycholic acid are among the bile acids that help the body absorb fat and control cholesterol levels. Although those particular bile acids have not been linked to AD before, another type, tauroursodeoxycholic acid, has been proposed as a possible anti-apoptotic therapeutic (Ramalho et al., 2008).
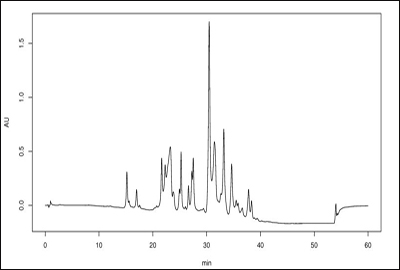
HPLC chromatograms line up peaks for each molecular component in a given mixture. (View larger image.) Image credit: Wikimedia Commons
Glycerophosphocholine, a precursor of the neurotransmitter acetylcholine, was another compound increased in AD samples. It has a long record in Alzheimer’s research: Levels are high in postmortem AD brains (Nitsch et al., 1992), and it has been previously reported as a potential CSF biomarker (Walter et al., 2004). In addition, the researchers observed that Alzheimer’s correlated with changes in D-glucosaminide, which is involved in sugar metabolism. If validated, it could become a new marker for AD.
In further studies, the researchers searched specifically for arachidonic acid, which has been suggested as an AD biomarker by the authors of a mouse study (Sanchez-Mejia et al., 2010). They found that the compound is boosted in the plasma of people with MCI, but not those with AD, differentiating the two, Legido-Quigley told ARF. In addition, the group is currently working on four molecules—of as-yet-unknown structure—that distinguish AD from controls with 99 percent accuracy, she told ARF. Legido-Quigley and her coauthors also noted that longitudinal studies are necessary, in particular to observe whether and when MCI morphs into AD.
Jules Griffin and colleagues at the University of Cambridge, U.K., used AD model mice to examine metabolomic changes in eight regions of the brain (Salek et al., 2010). Overall, they observed that affected animals evinced changes in certain amino acids and several molecules involved in fat or sugar metabolism. Griffin was particularly interested in the decrease in N-acetyl-L-aspartate (NAA) that the scientists observed in the sick mice. NAA’s function is not entirely clear, but neurons are chockfull of the stuff. Scientists suspect that it is involved in energy use, Griffin said, with well-fed neurons containing plenty of NAA, and sick or dying ones having less. The neurons in the AD mice “are having some problems in generating enough ATP for their processes, I suspect,” Griffin said. As one would expect from AD mice, the researchers observed metabolomic alterations in the hippocampus and cortex. They also noted changes in the cerebellum and midbrain, suggesting metabolism changes even in the regions not classically thought to be affected in AD.
“The thing that most interested me is, we were seeing metabolic changes before people were seeing changes in the histopathology,” Griffin said. “Before you actually see cell loss, you see metabolism being perturbed.” Imaging studies back up this assertion.
PET scans of glucose uptake are already regarded as a key marker for neural dysfunction in people with AD, and it might be an early marker at that (see ARF Webinar on Jack et al., 2010). For example, positron emission tomography (PET) scans show that glucose metabolism drops in ApoE4 carriers as early as their twenties and thirties (Reiman et al., 2004). The reduced glucose activity could indicate dysfunctional glucose metabolism or high activity at the synapses, said study author Eric Reiman, director of the Banner Alzheimer’s Institute in Phoenix, Arizona. Essentially, he said, the neurons “are wearing out the tread on their tires.” The researchers are following subjects longitudinally, looking for a link between glucose metabolism and future MCI or AD status. “We are pretty confident [glucose metabolism] is going to affect risk,” Reiman said, although he noted that the correlation only holds for groups, and may not predict decline in specific individuals.
More recently, Reiman’s group extended the genotype-glucose metabolism link to include Latino ApoE4 carriers in their fifties (Langbaum et al., 2010). In another study of postmortem tissue, young adult ApoE4 carriers evinced reduced mitochondrial activity in the brain, although they did not exhibit increases in amyloid-β or tau yet (Valla et al., 2010). “We think these mitochondrial changes might be some of the earliest changes you see with a predisposition to Alzheimer’s disease,” Reiman said.
The combination of imaging plus genomics, then, has proved to be a powerful pair (reviewed in Petrella et al., 2008). Could imaging be equally useful in metabolomics? Murali Doraiswamy of Duke University thinks it might, particularly with the adoption of nuclear magnetic resonance spectroscopy (MRS). “PET scans are limited in that they can only look at certain gross changes but cannot map detailed metabolite paths,” he wrote in an e-mail to ARF. When analyzing biochemical pathways by PET, he wrote, there are holes that the imaging cannot fill in, but MRS works with all kinds of markers. For example, MRS for hydrogen helps to differentiate AD from other dementias (Soher et al., 2005). “I think we are at a stage where it would be theoretically possible to use a combination of CSF metabolomics and PET/MRS to get to the bottom of this puzzle,” Doraiswamy wrote.
All these pilot experiments suggest that there is plenty of reason to study the metabolome in AD. The most exciting time in AD metabolomics is yet to come, Griffin said.—Amber Dance.
This is Part 3 of a four-part series. See also Part 1, Part 2, Part 4. View a PDF of the entire series.
References
News Citations
- Metabolomics: The Fourth Great Ome
- Metabolomics: Seeking Biomarkers for ALS, Parkinson’s, Huntington’s
- Metabolomics: All the Fish in the Sea
Webinar Citations
Paper Citations
- Kaddurah-Daouk R, Rozen S, Matson W, Han X, Hulette CM, Burke JR, Doraiswamy PM, Welsh-Bohmer KA. Metabolomic changes in autopsy-confirmed Alzheimer's disease. Alzheimers Dement. 2011 May;7(3):309-17. PubMed.
- Greenberg N, Grassano A, Thambisetty M, Lovestone S, Legido-Quigley C. A proposed metabolic strategy for monitoring disease progression in Alzheimer's disease. Electrophoresis. 2009 Apr;30(7):1235-9. PubMed.
- Ramalho RM, Viana RJ, Low WC, Steer CJ, Rodrigues CM. Bile acids and apoptosis modulation: an emerging role in experimental Alzheimer's disease. Trends Mol Med. 2008 Feb;14(2):54-62. PubMed.
- Nitsch RM, Slack BE, Wurtman RJ, Growdon JH. Release of Alzheimer amyloid precursor derivatives stimulated by activation of muscarinic acetylcholine receptors. Science. 1992 Oct 9;258(5080):304-7. PubMed.
- Walter A, Korth U, Hilgert M, Hartmann J, Weichel O, Fassbender K, Schmitt A, Klein J. Glycerophosphocholine is elevated in cerebrospinal fluid of Alzheimer patients. Neurobiol Aging. 2004 Nov-Dec;25(10):1299-303. PubMed.
- Sanchez-Mejia RO, Mucke L. Phospholipase A2 and arachidonic acid in Alzheimer's disease. Biochim Biophys Acta. 2010 Aug;1801(8):784-90. PubMed.
- Salek RM, Xia J, Innes A, Sweatman BC, Adalbert R, Randle S, McGowan E, Emson PC, Griffin JL. A metabolomic study of the CRND8 transgenic mouse model of Alzheimer's disease. Neurochem Int. 2010 Jul;56(8):937-47. PubMed.
- Jack CR, Knopman DS, Jagust WJ, Shaw LM, Aisen PS, Weiner MW, Petersen RC, Trojanowski JQ. Hypothetical model of dynamic biomarkers of the Alzheimer's pathological cascade. Lancet Neurol. 2010 Jan;9(1):119-28. PubMed.
- Reiman EM, Chen K, Alexander GE, Caselli RJ, Bandy D, Osborne D, Saunders AM, Hardy J. Functional brain abnormalities in young adults at genetic risk for late-onset Alzheimer's dementia. Proc Natl Acad Sci U S A. 2004 Jan 6;101(1):284-9. PubMed.
- Langbaum JB, Chen K, Caselli RJ, Lee W, Reschke C, Bandy D, Alexander GE, Burns CM, Kaszniak AW, Reeder SA, Corneveaux JJ, Allen AN, Pruzin J, Huentelman MJ, Fleisher AS, Reiman EM. Hypometabolism in Alzheimer-affected brain regions in cognitively healthy Latino individuals carrying the apolipoprotein E epsilon4 allele. Arch Neurol. 2010 Apr;67(4):462-8. PubMed.
- Valla J, Yaari R, Wolf AB, Kusne Y, Beach TG, Roher AE, Corneveaux JJ, Huentelman MJ, Caselli RJ, Reiman EM. Reduced posterior cingulate mitochondrial activity in expired young adult carriers of the APOE ε4 allele, the major late-onset Alzheimer's susceptibility gene. J Alzheimers Dis. 2010;22(1):307-13. PubMed.
- Petrella JR, Mattay VS, Doraiswamy PM. Imaging genetics of brain longevity and mental wellness: the next frontier?. Radiology. 2008 Jan;246(1):20-32. PubMed.
- Soher BJ, Doraiswamy PM, Charles HC. A review of 1H MR spectroscopy findings in Alzheimer's disease. Neuroimaging Clin N Am. 2005 Nov;15(4):847-52, xi. PubMed.
Other Citations
External Citations
Further Reading
Papers
- Cacabelos R. Pharmacogenomics and therapeutic strategies for dementia. Expert Rev Mol Diagn. 2009 Sep;9(6):567-611. PubMed.
- Orešič M, Lötjönen J, Soininen H. Systems medicine and the integration of bioinformatic tools for the diagnosis of Alzheimer's disease. Genome Med. 2010 Nov 15;2(11):83. PubMed.
- Barba I, Fernandez-Montesinos R, Garcia-Dorado D, Pozo D. Alzheimer's disease beyond the genomic era: nuclear magnetic resonance (NMR) spectroscopy-based metabolomics. J Cell Mol Med. 2008 Sep-Oct;12(5A):1477-85. PubMed.
- Watson AD. Thematic review series: systems biology approaches to metabolic and cardiovascular disorders. Lipidomics: a global approach to lipid analysis in biological systems. J Lipid Res. 2006 Oct;47(10):2101-11. PubMed.
- Zhang J, Goodlett DR, Montine TJ. Proteomic biomarker discovery in cerebrospinal fluid for neurodegenerative diseases. J Alzheimers Dis. 2005 Mar;8(4):377-86. PubMed.
News
- Scouting AD’s “Little League” Genes: Can Systems Biology Help?
- Metabolomics: The Fourth Great Ome
- Metabolomics: All the Fish in the Sea
- Ordnung, Please—Can Biomarkers Tame a Bewildering Overlap?
- HAI Seattle: Does Brain Amyloid Correlate With Sagging Metabolism?
- Lessons From the Lipidome—PLA2 Linked to AD Pathology
- Biomarker Roundup: Collecting Clues from MRIs to RNAs
Annotate
To make an annotation you must Login or Register.

Comments
No Available Comments
Make a Comment
To make a comment you must login or register.